Type 2 Diabetes: What You Need to Know Right Now
Type 2 diabetes is the most common form of diabetes worldwide. It means your body either doesn't make enough insulin or can't use the insulin it makes properly. The result? Higher blood sugar levels that can damage organs over time. The good news is you can keep those numbers in check with a few practical moves.
Everyday Steps to Keep Blood Sugar in Check
First, think about food. Choose whole grains, fresh veggies, lean proteins, and healthy fats. Cut back on sugary drinks, white bread, and large portions of processed snacks. A simple rule works: fill half your plate with non‑starchy veggies, a quarter with protein, and the rest with complex carbs.
Second, move a little every day. You don’t need a marathon – a brisk 30‑minute walk, a bike ride, or even dancing in the living room can boost insulin sensitivity. Try to break up long sitting periods; stand up, stretch, or do a quick set of squats.
Third, watch your sleep. Poor sleep messes with hormones that control hunger and blood sugar. Aim for 7‑9 hours of solid sleep, keep the room dark, and ditch screens an hour before bedtime.
Fourth, stay on top of stress. Stress hormones raise glucose levels, so practice relaxation techniques you enjoy – deep breathing, short meditation, or a hobby that makes you smile.
Finally, keep an eye on numbers. Check your blood sugar at home as recommended by your doctor, and note trends. If you see a pattern of high readings after certain meals or activities, adjust accordingly.
When to Talk to Your Doctor
Regular check‑ups are a must. If fasting blood sugar stays above 126 mg/dL, or your A1C (average sugar over three months) climbs above 6.5 %, it’s time for a deeper conversation. Your doctor can suggest medication, adjust dosages, or recommend a specialist.
Pay attention to symptoms that suddenly get worse: frequent urination, excessive thirst, blurry vision, or numbness in hands and feet. These could signal that your current plan needs tweaking.
Ask about newer medication options, such as GLP‑1 receptor agonists or SGLT2 inhibitors, especially if you have heart or kidney concerns. Many of these drugs help lower blood sugar while offering extra health benefits.
Don’t forget routine labs. Your doctor will want to see cholesterol, kidney function, and liver enzymes to catch any complications early.
Bottom line: type 2 diabetes is manageable. By eating smarter, moving regularly, sleeping well, handling stress, and staying connected with your healthcare team, you can keep blood sugar steady and enjoy a healthier life.
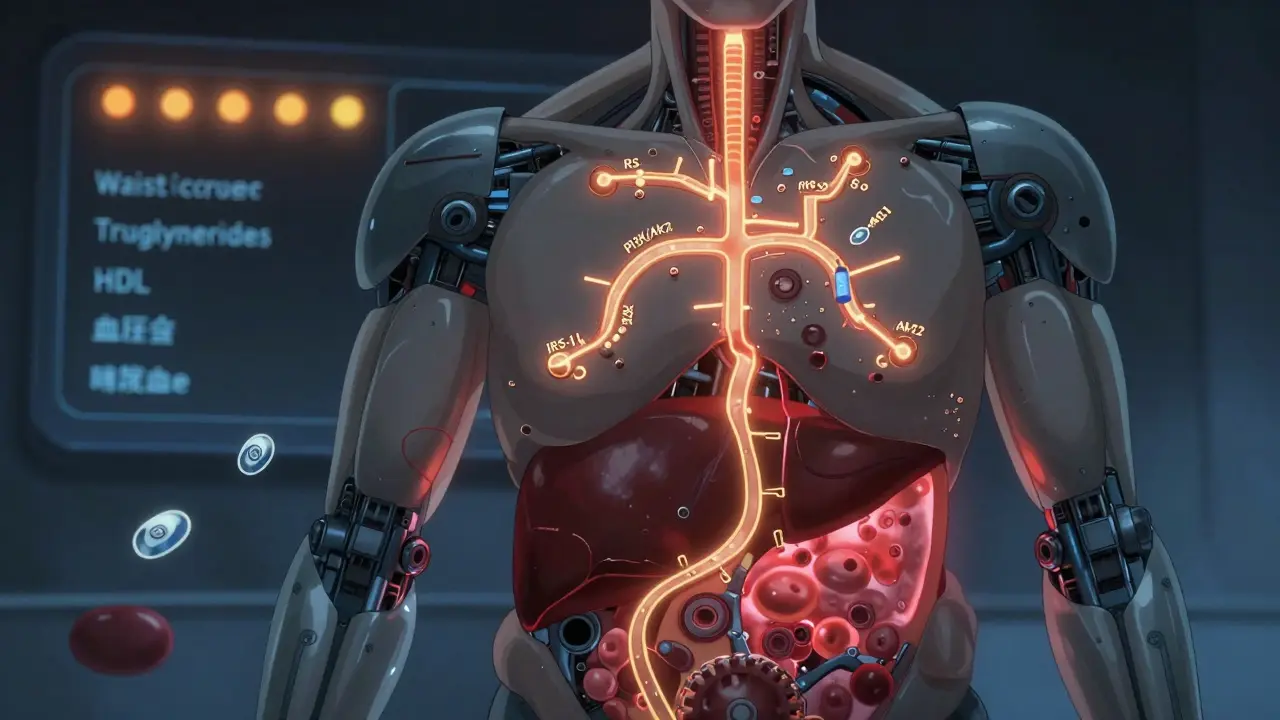
Type 2 Diabetes: Insulin Resistance and Metabolic Syndrome Explained
Feb, 17 2026Type 2 diabetes starts with insulin resistance, a hidden process that leads to metabolic syndrome. Learn how these conditions connect, why they’re dangerous, and what actually works to reverse them.
READ MORE
Diet-First Solutions: Replace or Reduce Metformin with Low-Carb, Mediterranean & Fasting Diets
Jul, 6 2025Explore how specific diet-first strategies like low-carb, Mediterranean, and intermittent fasting can help many reduce or avoid metformin use for type 2 diabetes management.
READ MORE