 Dec, 8 2025
Dec, 8 2025
When you take multiple medications, every pharmacy you visit becomes a potential blind spot in your safety net. If you fill your blood pressure pills at one store, your diabetes meds at another, and your pain relievers at a third, you’re not saving money-you’re risking your health. The truth is simple: using one pharmacy for all your prescriptions is one of the most effective ways to prevent dangerous drug interactions, avoid duplicate prescriptions, and stay in control of your health.
Why One Pharmacy Makes a Difference
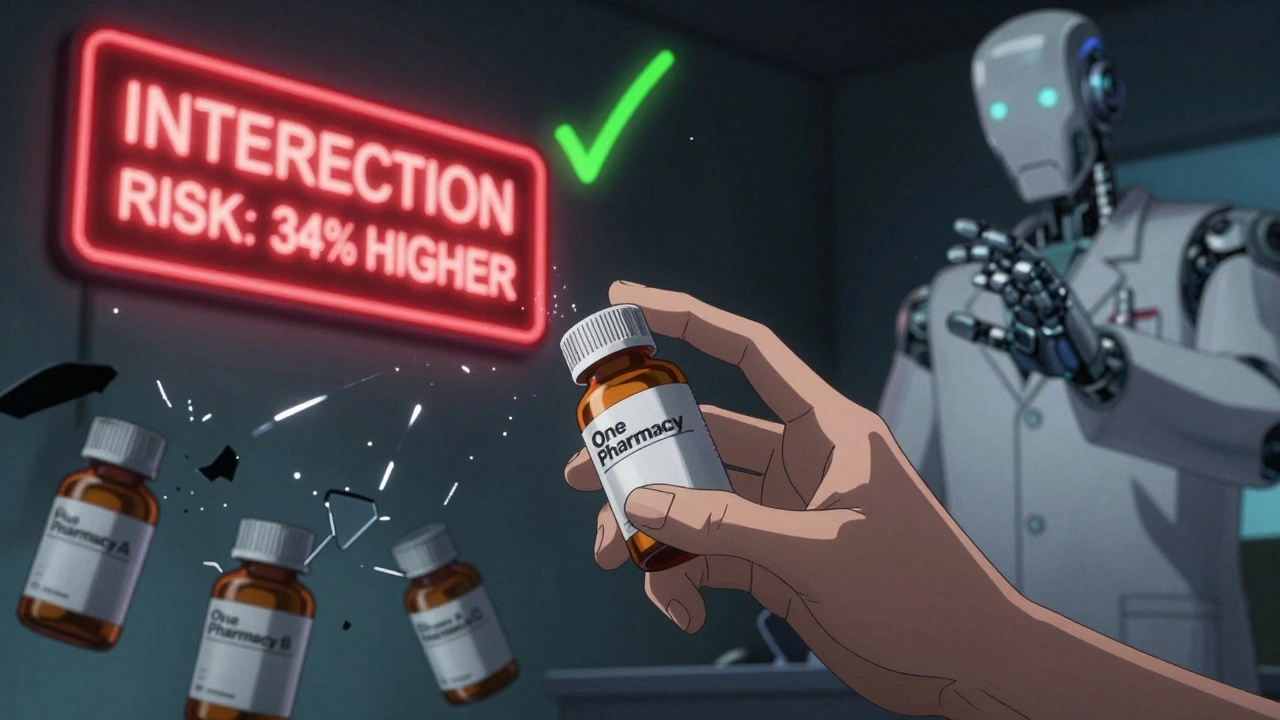
Pharmacists aren’t just dispensers of pills. They’re trained to spot hidden dangers in your medication list. When you use just one pharmacy, that pharmacist sees your full history: every prescription, over-the-counter drug, vitamin, and herbal supplement. That complete picture lets them catch interactions before they happen. Consider this: a 2014 study published in the Journal of Managed Care & Specialty Pharmacy found that people using multiple pharmacies had a 34% higher risk of dangerous drug-drug interactions than those who stuck with one. One of the most common and deadly combinations? Warfarin (a blood thinner) and NSAIDs like ibuprofen. Together, they can cause serious internal bleeding-five times more likely than with warfarin alone. If two different pharmacies fill those prescriptions, neither pharmacist may know the other has it. But if both are at the same pharmacy, the system flags it immediately.How Drug Interaction Systems Work
Modern pharmacy software doesn’t just count pills. It scans your entire medication list against a database of over 10,000 known drug interactions. When a new prescription comes in, the system checks it against everything else you’re taking. If there’s a red flag-say, mixing antidepressants that raise serotonin too high-the pharmacist gets an alert. But here’s the catch: if your meds are scattered across three pharmacies, the system only sees a third of your history. That’s why pharmacists override about 80% of alerts when patients use multiple locations-they assume the system is missing data. That’s not confidence. That’s guesswork. And guesswork kills. At a single pharmacy, the system works as intended. Your pharmacist sees everything. That’s why therapy duplication-taking two pills with the same active ingredient-drops from 7% in multi-pharmacy users to just 0.3% in those who consolidate. That’s not a small difference. That’s the difference between a headache and a hospital stay.Med Sync: More Than Just Convenience
Many pharmacies now offer medication synchronization, or “med sync.” It’s not just about getting all your refills on the same day. It’s a safety system wrapped in convenience. Here’s how it works:- You meet with your pharmacist for a full review of every medication you take.
- They adjust refill dates by giving you short-term fills to line everything up.
- From then on, all your prescriptions are ready for pickup on the same day each month.
- You get a quick check-in with your pharmacist every time you pick up.

The Cost Trap: Why People Use Multiple Pharmacies
Let’s be honest: price matters. A 2023 analysis by SingleCare found that 63% of people use multiple pharmacies to save money-sometimes $150 to $300 a year. That’s real cash. But here’s what those savings don’t show you: The same study found that people using multiple pharmacies have a 27% higher risk of an adverse drug event. The average cost of one preventable hospitalization from a drug interaction? $8,750. That’s 30 times more than the annual savings from price shopping. And it’s not just about money. It’s about stress. A 2022 survey by Avalon Pharmacy found that 41% of people using multiple pharmacies missed at least one dose each month because they couldn’t keep track of which pill went where. That’s not forgetfulness. That’s fragmentation.Real Stories, Real Risks
There’s a reason the Cleveland Clinic documented a case of serotonin syndrome from conflicting antidepressant prescriptions filled at two different pharmacies. Serotonin syndrome can cause seizures, high fever, and even death. It doesn’t happen because someone was careless. It happens because two pharmacists didn’t know what the other was dispensing. On Reddit’s r/Pharmacy subreddit, 68% of 142 respondents said they’d recommend using one pharmacy if you take three or more medications. But 55% admitted they still juggle pharmacies because of price. That tension-between safety and savings-is real. But it’s not a trade-off you should make.How to Make the Switch
Switching to one pharmacy doesn’t require a miracle. Here’s how to do it in 2-4 weeks:- Write down every medication you take-prescription, OTC, supplements, vitamins. Don’t skip anything.
- Call your current pharmacy and ask them to transfer all your prescriptions to your chosen pharmacy. Transfers usually take 2-5 business days.
- Ask for a med sync enrollment. Most pharmacies will schedule a 30-45 minute review with you.
- During the review, ask: “Are any of these medications interacting? Is anything redundant?”
- Once synced, keep your medication list updated. Bring it to every doctor’s appointment.
What’s Changing Now
Electronic health records (EHRs) like Epic and Cerner now share medication data across providers. That helps-but it doesn’t fix the problem. Not all pharmacies are connected. Not all doctors update records in real time. And not all patients give permission for data sharing. The real solution? A single pharmacy that knows you. That remembers your allergies. That knows you can’t swallow pills without water. That notices you’ve been picking up your blood pressure med less often and calls to ask why. That’s not technology. That’s care.Who Benefits Most?
You don’t have to be elderly or chronically ill to benefit. But if you take five or more medications, you’re in the highest-risk group. According to the University of Southern California, 15% of U.S. adults fall into that category-and that number is rising. People with diabetes, heart disease, kidney issues, depression, or arthritis are especially vulnerable. Their regimens are complex. Their margins for error are thin. One wrong pill can send them to the ER. But even younger people on a few meds can benefit. If you’re on an antibiotic, a painkiller, and a sleep aid, your pharmacist still needs to see all three to make sure they don’t clash.Final Thought: Safety Isn’t Optional
Choosing one pharmacy isn’t about loyalty. It’s about survival. It’s about making sure the person handing you your pills knows what else you’re taking. It’s about preventing a mistake that could end your day-or your life. You wouldn’t drive a car with half your brakes checked. Don’t manage your health with half your meds tracked. Consolidate your prescriptions. Get on med sync. Talk to your pharmacist. Ask the questions. Keep your list updated. It’s not complicated. It’s just critical.Can I use one pharmacy if I have insurance from different providers?
Yes. Your insurance doesn’t limit which pharmacy you use. Most pharmacies accept multiple insurance plans. If your current pharmacy doesn’t accept one of your plans, call other pharmacies in your area and ask. Many will work with you to find a solution. The key is to consolidate all your prescriptions at one location, even if you’re paying out-of-pocket for some. The safety benefit outweighs the inconvenience.
What if my pharmacy doesn’t offer med sync?
Ask them to start. Many pharmacies don’t advertise med sync unless patients request it. If they say no, consider switching to one that does. CVS, Walgreens, Rite Aid, and most independent pharmacies now offer it. You can also ask your doctor or local health department for recommendations. Med sync is now a standard service, not a special perk.
Should I include over-the-counter meds and supplements in my list?
Absolutely. Many dangerous interactions happen with common OTC drugs like ibuprofen, antacids, or melatonin. Herbal supplements like St. John’s Wort can interfere with antidepressants, blood thinners, and birth control. Your pharmacist needs to see the full picture-including everything you take, even if you think it’s harmless.
How often should I update my medication list?
Update it every time you start, stop, or change a medication-even if it’s temporary. Keep a printed copy in your wallet and a digital copy on your phone. Review it with your pharmacist every time you pick up your prescriptions. Don’t wait for your annual checkup. Changes happen fast, and your pharmacist can’t protect you if they don’t know.
Is this only for older adults?
No. While older adults are more likely to take multiple medications, younger people on antidepressants, birth control, pain meds, or chronic condition treatments are also at risk. Anyone taking three or more medications should use one pharmacy. The risk of interaction doesn’t care about your age-it cares about what’s in your body.
Elliot Barrett
December 10, 2025 AT 04:39Yeah sure, one pharmacy sounds great in theory. But try getting your $200/month insulin covered when your pharmacy only takes one insurance and you’re stuck paying $400 out of pocket. Safety’s nice, but so is not choosing between food and meds.
Maria Elisha
December 10, 2025 AT 17:19I switched to one pharmacy last year and my pharmacist caught that my blood pressure med was canceling out my kidney med. She called my doctor same day. No hospital trip. No drama. Just someone who actually knows what’s in my body. Why is this even a debate?
Anna Roh
December 12, 2025 AT 14:49People act like this is some revolutionary idea but it’s literally basic healthcare hygiene. You wouldn’t use three different dentists and expect them to coordinate your cavities, so why do it with pills? I’ve been doing this since I started on five meds at 32. My pharmacist remembers my cat’s name and that I hate blue capsules. That’s not service. That’s care.
Also, med sync? Life-changing. I used to forget half my pills because I had five different pickup days. Now? One day a month. I even started taking my vitamins again. Who knew convenience could save your life?
And yes, include every damn supplement. St. John’s Wort with my antidepressant almost sent me to the ER. My pharmacist flagged it. The other one? Silent. That’s not luck. That’s system.
Stop treating your meds like a grocery list. They’re not interchangeable. They’re not optional. They’re the reason you’re still here.
om guru
December 13, 2025 AT 06:10Katherine Chan
December 13, 2025 AT 23:35Shubham Mathur
December 15, 2025 AT 10:35Katherine Rodgers
December 15, 2025 AT 15:48Guylaine Lapointe
December 16, 2025 AT 03:48It’s not just about drug interactions. It’s about accountability. When your prescriptions are scattered, no one is responsible. When they’re consolidated, someone has to care. That’s the difference between a system and a void. You don’t get to outsource your health to convenience. You owe it to yourself to be seen. To be known. To be protected.
And if your pharmacy doesn’t offer med sync? You’re not being served. You’re being ignored. That’s not your fault. But it’s your responsibility to demand better.
Sarah Gray
December 17, 2025 AT 03:43How quaint. You think your pharmacist is your therapist? I’ve seen pharmacists who can’t tell the difference between lisinopril and losartan. This isn’t care. It’s a marketing gimmick wrapped in emotional manipulation. And don’t get me started on med sync. It’s just a way for CVS to get you in the door so they can upsell you protein powder and essential oils.
Suzanne Johnston
December 17, 2025 AT 13:32There’s a deeper truth here. We’ve turned healthcare into a transaction. We shop for pills like we shop for socks. But medicine isn’t about price. It’s about presence. The pharmacist who knows your name, your allergies, your dog’s name, and the fact that you skip your pills on weekends-that’s not a service. That’s a relationship. And relationships can’t be optimized. They can only be honored.
Maybe the real problem isn’t the pharmacies. It’s that we’ve forgotten how to be patients.
William Umstattd
December 18, 2025 AT 02:07My uncle died from a drug interaction. Two pharmacies. Two pharmacists. Zero communication. He was 58. He had a daughter in college. He didn’t die from cancer. He died because no one bothered to connect the dots. Don’t be the person who says ‘I didn’t know’ after it’s too late. This isn’t advice. This is a warning.
Angela R. Cartes
December 18, 2025 AT 20:50My pharmacist is literally the only person who knows what I take. I told her I was taking turmeric for inflammation. She said ‘oh you’re on warfarin? That’s like playing Russian roulette with your brain.’ I cried. Then I switched. Now I bring her cookies. She’s my hero. 🥺
Andrea Beilstein
December 19, 2025 AT 09:53In my village in Nepal, we used to take all our herbs and remedies to the same elder healer. He knew what each plant did, who was allergic, who was pregnant, who was grieving. He didn’t need a computer. He had memory. He had presence. We’ve outsourced that to algorithms and insurance networks. But the human touch? That’s still the only thing that saves lives.
One pharmacy isn’t about efficiency. It’s about remembering that you’re not a data point. You’re a person.