 Dec, 19 2025
Dec, 19 2025
Every year, over 23,000 people end up in the emergency room because of something most people don’t even think twice about: taking a supplement with their medicine. It’s not rare. It’s not unusual. It’s happening to people who think they’re being careful - the kind of people who read labels, eat well, and try to stay healthy. But here’s the problem: supplement and medicine interactions aren’t listed on the bottle. No warning sticker. No fine print. And most doctors don’t ask.
Why Your Supplement Could Be Dangerous
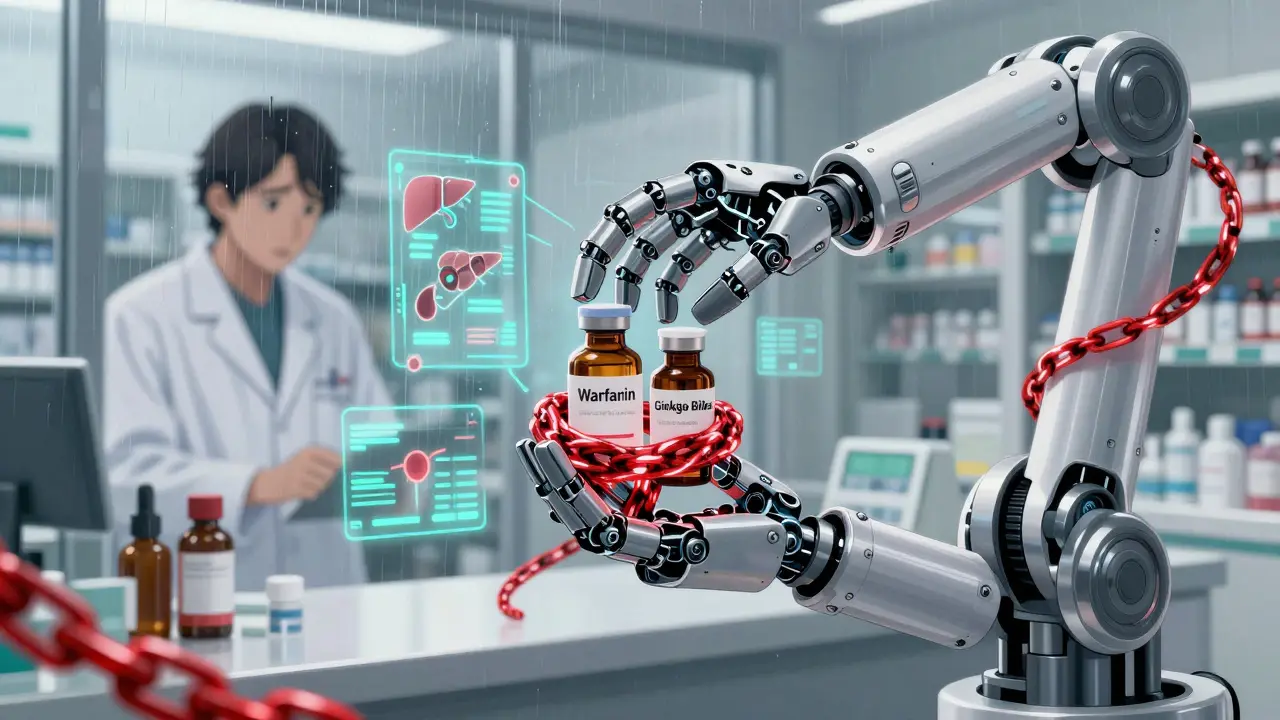
You might think, "It’s natural, so it’s safe." That’s the biggest myth in the supplement world. Natural doesn’t mean harmless. St. John’s wort, for example, is a plant. People take it for mood support. But it’s also one of the most dangerous supplements you can mix with prescription drugs. It doesn’t just cause mild side effects. It can make your birth control fail. It can drop your HIV medication levels by over half. It can cause your transplant organ to be rejected. How? Because it forces your liver to break down other drugs faster - sometimes so fast that they stop working entirely. In one study, organ transplant patients taking St. John’s wort saw their cyclosporine levels drop by 50-60%. That’s not a small change. That’s life-threatening. Even something as simple as vitamin E can be risky. If you’re on warfarin (a blood thinner), taking more than 400 IU a day of vitamin E can increase your bleeding risk by 25-30%. Ginkgo biloba? It can raise your INR - a measure of how long your blood takes to clot - by 2.5 to 3.5 times in some people. That’s not a typo. That’s bleeding you didn’t plan for.What You Need to Ask Before Taking Anything
You don’t need to be a scientist to protect yourself. You just need to ask the right questions - before you swallow that pill.- Does this supplement affect how your body processes your medicine? Many supplements work by changing the activity of liver enzymes - especially CYP3A4 and P-glycoprotein. St. John’s wort turns these enzymes on full blast, flushing drugs out of your system. Other supplements, like grapefruit juice, do the opposite - they slow things down, causing dangerous buildup. If you’re on statins, antidepressants, blood pressure meds, or immunosuppressants, this matters.
- Could this make your medicine stronger or weaker? Ginkgo biloba and garlic supplements can amplify the effects of blood thinners. That’s not a bonus - it’s a risk. On the flip side, milk thistle might help protect your liver during chemotherapy, but only if you’ve talked to your oncologist first. Some supplements interfere with cancer drugs in ways that reduce their effectiveness. You don’t want to be the person who took a supplement thinking it helped - and accidentally made your treatment fail.
- Has this supplement been studied with my exact medication? Only about 15% of supplements have any real clinical data on interactions. That means for most of what’s on the shelf, we’re guessing. If your doctor says, "I don’t know," that’s not an answer. It’s a red flag. Don’t guess. Wait. Ask for alternatives.
- Are there safer versions? Not all ginseng is the same. Asian ginseng can raise blood pressure and interfere with blood thinners. American ginseng? Much lower risk. Same with echinacea - some forms trigger immune reactions that can mess with autoimmune drugs. Know the difference.
- What symptoms should I watch for? If you start feeling dizzy, confused, have a rapid heartbeat, or feel unusually stiff or twitchy after starting a supplement, stop it immediately. These could be signs of serotonin syndrome - a dangerous condition caused by mixing supplements like St. John’s wort with antidepressants. It’s rare, but it kills. And it happens faster than you think.
- Is there a reason I’m taking this at all? Many people take supplements because they heard it "helps immunity" or "boosts energy." But do you actually need it? For most healthy adults, a balanced diet covers everything. Supplements aren’t vitamins - they’re active substances. Treat them like medicine.
- Have I told my pharmacist? Pharmacists are the unsung heroes of drug safety. They see your full prescription list. They know what interacts with what. And they’re trained to ask about supplements. Yet, only 32% of primary care doctors even document supplement use in your chart. Your pharmacist might be your best line of defense.
Who’s at the Highest Risk?
Some people are walking into danger without even knowing it. If you’re on:- Warfarin or other blood thinners - avoid ginkgo, garlic, vitamin E (high doses), and ginger supplements. Your INR can spike without warning.
- Immunosuppressants like cyclosporine or tacrolimus - St. John’s wort, black cohosh, and echinacea can trigger organ rejection. One in seven transplant rejections is linked to supplements.
- HIV medications - St. John’s wort cuts drug levels so low that the virus can rebound. That’s not just risky - it’s a public health emergency.
- Birth control - St. John’s wort reduces effectiveness by 40-50%. Women have gotten pregnant because no one told them.
- Cancer treatments - Many antioxidants (like high-dose vitamin C or E) can interfere with chemo and radiation. They’re not helping. They’re hurting.
The System Isn’t Designed to Protect You
The FDA doesn’t approve supplements before they hit the shelves. Unlike pills you get from your doctor, supplements don’t need to prove they’re safe or effective. They just need to be labeled "dietary supplement." There are over 85,000 supplement products on the market right now. Less than 3% have any documented interaction data. And 70% of labels get the ingredient amounts wrong - meaning you might think you’re taking 500 mg of something, but you’re actually getting 1,200 mg. Or none at all. Pharmacists are catching on. Nearly 9 out of 10 now check for supplement interactions during medication reviews. But only 1 in 3 doctors even ask. You’re the only one who can bridge that gap.
What You Can Do Right Now
1. Make a list - Write down every supplement, herb, vitamin, and mineral you take. Include dosage and frequency. 2. Bring it to your next appointment - Don’t wait for them to ask. Hand them the list. Say, "I want to make sure these are safe with my meds." 3. Talk to your pharmacist - They can run a free interaction check in minutes. Most will do it without an appointment. 4. Use trusted resources - The NIH’s Office of Dietary Supplements and the LiverTox database have reliable, science-backed info. Avoid blogs, Instagram influencers, and supplement company websites. 5. Stop if you feel off - If you start feeling strange after adding something new - even if it’s "natural" - stop it. Write down what you took and when symptoms started. Report it to the FDA’s MedWatch program.It’s Not About Fear - It’s About Control
You’re not being paranoid. You’re being smart. The supplement industry makes billions selling hope. But your health isn’t a gamble. You don’t need to avoid supplements forever. You just need to know when they’re safe - and when they’re not. The truth is, some supplements are fine. Milk thistle, when used under supervision, can help protect the liver during cancer treatment. Vitamin D, if you’re deficient, is essential. But none of that matters if you’re mixing them without knowing the risks. You don’t need to be an expert. You just need to ask the questions. And then listen - really listen - to the answers.Can I take vitamin D with my blood pressure medicine?
Yes, vitamin D is generally safe with most blood pressure medications. There’s no strong evidence it interferes with ACE inhibitors, beta-blockers, or calcium channel blockers. However, if you’re taking thiazide diuretics (like hydrochlorothiazide), high doses of vitamin D can raise calcium levels too much, potentially causing kidney stones or heart rhythm issues. Stick to the recommended dose (600-800 IU daily) unless your doctor says otherwise.
Is St. John’s wort ever safe to use?
Almost never if you’re on any prescription medication. It interacts with over 50 common drugs, including antidepressants, birth control, HIV meds, transplant drugs, and heart medications. Even if you think you’re only taking one med, many people take multiple pills without realizing how they interact. The risk far outweighs any potential benefit. If you need help with depression, talk to your doctor about FDA-approved options.
Why don’t doctors warn me about supplements?
Most doctors have 15 minutes per appointment. They’re trained to focus on diagnosing and treating illness - not supplement safety. Only 1.2 minutes of that time is typically spent on supplements, according to a JAMA study. Many also assume patients will mention them. They don’t. And because supplements aren’t regulated like drugs, doctors often don’t have clear data to reference. That’s why you need to bring the list and ask.
Are "clinical-grade" or "pharmaceutical-grade" supplements safer?
These terms have no legal meaning. The FDA doesn’t recognize them. A supplement labeled "pharmaceutical-grade" could still be contaminated, mislabeled, or interact dangerously. The only reliable certification is USP Verified - look for the USP mark on the bottle. It means the product was tested for purity, strength, and consistency. Even then, interaction data isn’t guaranteed.
Can I just stop my supplement before surgery?
Not always. Some supplements, like ginkgo, garlic, and fish oil, can increase bleeding risk for days or even weeks after you stop taking them. If you’re having surgery, tell your surgeon and anesthesiologist about every supplement you take - even if you think it’s harmless. Most hospitals now require you to stop all supplements at least 1-2 weeks before surgery. Don’t assume they’ll know.
What should I do if I think I had a bad reaction?
Stop the supplement immediately. Contact your doctor or go to the ER if you have symptoms like rapid heartbeat, confusion, chest pain, unusual bleeding, or severe dizziness. Then report it to the FDA’s MedWatch program at fda.gov/medwatch. This helps track dangerous interactions and protect others. You’re not just helping yourself - you’re helping prevent someone else’s emergency.
Adrienne Dagg
December 19, 2025 AT 16:04Sajith Shams
December 21, 2025 AT 11:51shivam seo
December 23, 2025 AT 01:20Andrew Kelly
December 23, 2025 AT 02:40Isabel Rábago
December 23, 2025 AT 05:10Matt Davies
December 24, 2025 AT 10:23Mike Rengifo
December 24, 2025 AT 23:58Dev Sawner
December 26, 2025 AT 02:45Moses Odumbe
December 27, 2025 AT 00:57Meenakshi Jaiswal
December 28, 2025 AT 10:04