 Nov, 13 2025
Nov, 13 2025
Quercetin Medication Interaction Checker
Check Your Medication Risk
Enter your medication name to see if it interacts with quercetin supplements. Quercetin can block liver enzymes (CYP3A4, CYP2D6, CYP2C19) that process many drugs, potentially increasing drug levels by 20% to over 300%.
Interaction Results
Many people take quercetin supplements hoping to reduce inflammation, boost immunity, or fight allergies. But what they don’t realize is that this popular flavonoid can quietly change how their medications work-sometimes dangerously. If you’re on any prescription drugs, especially blood thinners, heart meds, or cancer treatments, taking high-dose quercetin could be putting you at risk.
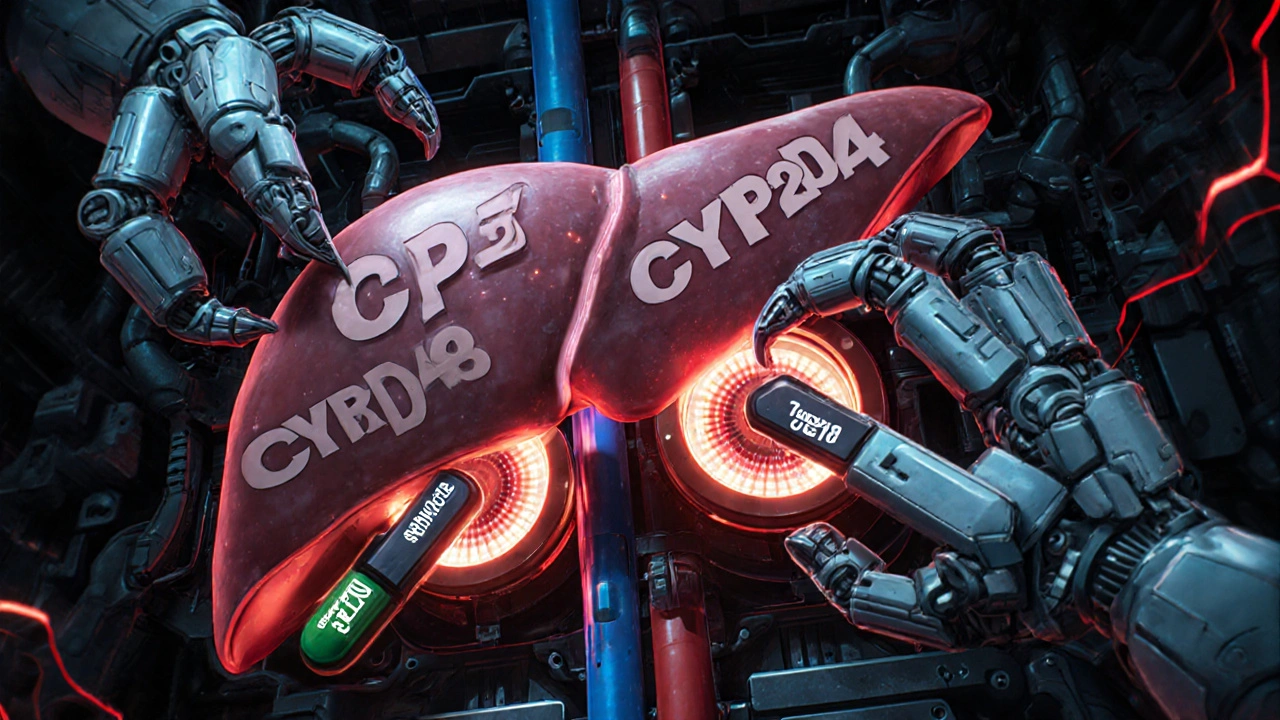
What Quercetin Does to Your Liver’s Drug-Cleaning System
Your body uses enzymes in the liver and gut to break down most medications. The most important ones are called CYP enzymes-CYP3A4, CYP2D6, and CYP2C19. These are like molecular scissors that chop up drugs so your body can get rid of them. Quercetin doesn’t just pass through your system. It gets in the way.
Studies show quercetin blocks these enzymes, especially at doses above 500 mg per day. In lab tests, it inhibits CYP3A4 by 40-60%, CYP2D6 by 70-85%, and CYP2C19 by 40-60%. That means drugs that normally get cleared quickly now stick around longer. Their levels in your blood can rise by 20% to over 300%, depending on the medication.
Think of it like this: if your body usually clears a drug in 4 hours, quercetin might stretch that to 8 or 12 hours. The drug keeps working, and you might not even know why you’re feeling dizzy, nauseous, or unusually tired.
Medications That Can Become Dangerous with Quercetin
Not all drugs are affected the same way. Some are especially risky when mixed with quercetin because they have a narrow safety window-small changes in blood levels can cause serious harm.
- Warfarin (Coumadin): Quercetin can raise INR levels by 0.8 to 1.5 points, pushing you into dangerous bleeding territory. One case report linked a 78-year-old man’s unexplained bruising and nosebleeds to quercetin use while on warfarin.
- Abemaciclib and other cancer drugs: Used for breast cancer, these drugs are metabolized by CYP3A4. Quercetin can increase their blood levels by 25-35%, raising the risk of severe diarrhea, low white blood cell counts, and fatigue.
- Cyclosporine and tacrolimus: These transplant drugs must stay in a very tight range. Quercetin can push trough levels up by 30-50%, leading to kidney damage or nerve problems.
- Acenocoumarol and other vitamin K antagonists: Similar to warfarin, these anticoagulants become harder to control when quercetin is in the mix.
- Apixaban and rivaroxaban (DOACs): Even newer blood thinners aren’t safe. Quercetin blocks transporters like OATP1B1 and BCRP, which help move these drugs out of the body. That means higher exposure and higher bleeding risk.
- Statins like simvastatin: Increased levels can cause muscle damage (rhabdomyolysis), which can lead to kidney failure.
- Antidepressants like sertraline and fluoxetine: These are processed by CYP2D6. Quercetin can make them too strong, causing serotonin syndrome-agitation, rapid heart rate, fever, and confusion.
Why Food Isn’t the Problem-But Supplements Are
You might be thinking: ‘I eat apples, onions, and broccoli every day. Why is that okay but supplements aren’t?’
Good question. The quercetin in food is bound to sugar molecules (glycosides), like rutin. Your body absorbs it slowly, and only a tiny fraction becomes active. A cup of onions gives you about 10-30 mg of quercetin. Even a large apple has less than 10 mg.
Supplements, on the other hand, deliver 500 mg to 1,000 mg in one pill. That’s 50 to 100 times more than you’d get from diet. And here’s the catch: the aglycone form (free quercetin) in supplements is the one that strongly inhibits enzymes. That’s the form that shuts down your liver’s drug-processing system.
Studies show quercetin glycosides (like those in food) are only about 30-40% as potent as the pure form in pills. So yes, your diet is fine. Your supplement? Not so much.
Who’s Most at Risk?
Not everyone who takes quercetin will have a problem. But some groups are far more vulnerable.
- People over 65: Liver and kidney function decline with age. Studies show older adults clear quercetin metabolites 25-40% slower, meaning it builds up faster and lasts longer.
- People on multiple medications: If you’re taking 5 or more drugs, you’re more likely to be on one that interacts with quercetin. Polypharmacy is the silent killer here.
- People with liver disease: If your liver is already struggling, adding an enzyme blocker like quercetin can push it into failure.
- People with cancer or transplants: These patients rely on precise drug levels. Even a 20% change can mean the difference between treatment working and failing.
The European Food Safety Authority (EFSA) warned in 2018 that doses over 1,000 mg/day pose ‘potential concerns’ for drug interactions. The FDA agrees. In its 2020 draft guidance, it listed quercetin as a dietary supplement of concern for interaction studies.
What You Should Do Right Now
If you’re taking quercetin supplements and any prescription medication, don’t panic-but do act.
- Check your meds. Look up your drugs on a reliable interaction checker (like Medscape or Micromedex). If they’re metabolized by CYP3A4, CYP2D6, or CYP2C19, you’re at risk.
- Stop high-dose quercetin. If you’re taking more than 500 mg per day, cut it in half-or better yet, stop entirely until you talk to your doctor.
- Don’t rely on ‘natural’ labels. Just because it’s sold as a supplement doesn’t mean it’s safe with your meds. The FDA doesn’t test supplements for interactions before they hit shelves.
- Ask your pharmacist. Pharmacists are trained to spot these interactions. Bring your supplement bottle to your next visit. They’ll tell you if it’s risky.
- If you must take it, space it out. Some studies suggest taking quercetin 4-6 hours apart from your medication can reduce interaction risk by 30-50%. But this isn’t foolproof. It’s a band-aid, not a solution.
The Bigger Picture: Why This Keeps Happening
Quercetin isn’t the only supplement that does this. Grapefruit, St. John’s wort, green tea extract, and curcumin all interfere with drug metabolism. But quercetin is unique because it hits multiple enzymes and transporters at once.
And here’s the problem: supplement companies aren’t required to prove safety before selling. The Dietary Supplement Health and Education Act of 1994 lets them market anything without FDA approval. Since 2018, the FDA has sent 17 warning letters to quercetin brands for making illegal claims about curing cancer or reversing heart disease.
Meanwhile, sales of quercetin supplements hit $387 million in 2022. About 18 million Americans take them. And 42% of users take more than 500 mg per day. That’s a lot of people unknowingly mixing a potent enzyme blocker with life-saving drugs.
The FDA is working on new labeling rules for 2024 that would require warnings about drug interactions on high-risk supplements. But until then, the burden is on you.
Bottom Line: Your Health Isn’t a Guessing Game
Quercetin isn’t evil. It’s a natural compound with real benefits. But when you take it in pill form at high doses, it stops being a health aid and starts being a drug-interaction hazard.
If you’re on any medication-especially blood thinners, cancer drugs, heart meds, or antidepressants-quercetin supplements are not worth the risk. The data is clear. The warnings are out there. The cases are documented.
Your body doesn’t know the difference between a supplement and a drug. It only knows what’s in your bloodstream. And if quercetin is there, it’s changing how everything else works.
Don’t assume it’s safe because it’s natural. Don’t trust marketing claims. Talk to your doctor. Or better yet, talk to your pharmacist. They’re the ones who catch these hidden dangers before they become emergencies.
Can I still eat foods high in quercetin like onions and apples?
Yes. The quercetin in whole foods like onions, apples, berries, and broccoli is bound to sugars and absorbed slowly. Your body processes it in a way that doesn’t significantly block drug-metabolizing enzymes. You’d need to eat dozens of apples or pounds of onions daily to reach the levels that cause interactions-something no one does. Supplements are the problem, not your diet.
How do I know if my medication interacts with quercetin?
Check if your drug is metabolized by CYP3A4, CYP2D6, or CYP2C19 enzymes. Common ones include warfarin, statins, antidepressants, blood pressure meds like amlodipine, and cancer drugs like abemaciclib. You can search your medication name on databases like Medscape’s Drug Interactions Checker or ask your pharmacist. If it’s on that list, avoid quercetin supplements.
Is 250 mg of quercetin safe with my meds?
It depends. Even 250 mg can cause interactions in sensitive people, especially older adults or those on multiple drugs. The 500 mg/day threshold is a general guideline, not a safe limit. If you’re on a narrow-therapeutic-index drug like warfarin, cyclosporine, or a cancer drug, even 100 mg could be risky. When in doubt, skip it.
I’ve been taking quercetin with my blood thinner. Should I get tested?
Yes. If you’re on warfarin, check your INR level immediately. If you’re on a DOAC like apixaban or rivaroxaban, ask your doctor about drug level monitoring (though it’s not routinely done). Watch for signs of bleeding: unusual bruising, nosebleeds, blood in urine or stool, or headaches that won’t go away. Stop the supplement and call your doctor right away if you notice any of these.
Are there safer alternatives to quercetin for inflammation?
Yes. Omega-3 fatty acids (fish oil), curcumin (in low doses, under 500 mg), and ginger extract have anti-inflammatory effects without the same enzyme-blocking risks. But even these can interact with blood thinners, so always check with your pharmacist before starting anything new. Lifestyle changes-like reducing sugar, getting more sleep, and moving daily-are often the safest and most effective way to reduce inflammation.
Sean Hwang
November 13, 2025 AT 02:40Man, I took quercetin for months thinking it was just a fancy apple extract. Didn’t even know it could mess with my statin. Thanks for the wake-up call. Stopped it yesterday.
Brittany C
November 13, 2025 AT 08:16As a clinical pharmacist, I see this every week. Patients read ‘natural’ and assume ‘safe.’ The CYP enzyme inhibition data is rock solid. Quercetin isn’t the villain-it’s the silent saboteur. Always ask: ‘What’s the mechanism?’ Not ‘Is it organic?’
Ryan Anderson
November 14, 2025 AT 21:09Just shared this with my dad-he’s on warfarin and took 500mg daily ‘for immunity.’ He’s freaking out now. Seriously, if you’re on meds, don’t gamble with supplements. Your pharmacist isn’t just there for refills.
Barry Sanders
November 15, 2025 AT 08:28Another ‘natural’ supplement cultist spreading fear. Quercetin is fine. If you’re on 12 meds and take pills like candy, that’s your problem-not the supplement.
gent wood
November 16, 2025 AT 06:36I know this sounds dramatic, but please-don’t ignore this. I had a friend develop internal bleeding after mixing quercetin with apixaban. He didn’t even know they could interact. It’s not fearmongering. It’s pharmacology.
Anjan Patel
November 17, 2025 AT 19:52Look, I get it. Big Pharma hates natural remedies. But here’s the truth: your liver doesn’t care if it’s a pill or a plant. If it blocks enzymes, it’s a drug. And if you’re on anticoagulants or cancer meds? You’re playing Russian roulette with your liver.
Scarlett Walker
November 18, 2025 AT 06:19I used to take 1000mg daily for ‘anti-aging.’ Now I eat onions and berries instead. No more weird fatigue. No more weird INR spikes. Sometimes the simplest fix is the best one.
Hrudananda Rath
November 20, 2025 AT 00:10It is, without a shadow of a doubt, a profound and deeply concerning pharmacological phenomenon. The regulatory vacuum surrounding dietary supplements-particularly those with potent enzyme-modulating properties-is nothing short of scandalous. One cannot help but wonder whether the FDA's inaction constitutes a dereliction of duty. The data is irrefutable. The consequences, catastrophic. And yet, the market thrives.
Sean Evans
November 20, 2025 AT 10:12LOL at people saying ‘just eat onions.’ You think your 30mg from an apple is safe? Nah. You’re just a sheep. I’ve been taking 1000mg for 3 years with my blood pressure med. No issues. 🤷♂️💊 #NaturalIsBetter
Scott Saleska
November 20, 2025 AT 16:43Actually, the 2020 FDA draft guidance specifically flagged quercetin for interaction studies because of its dual inhibition of CYP3A4 and OATP1B1. You can’t just dismiss this as ‘Big Pharma fear.’ The science is peer-reviewed. The case reports are real. And yes, even 250mg can matter in elderly patients on multiple meds.
Ashley Durance
November 22, 2025 AT 06:10Everyone’s panicking over quercetin. Meanwhile, they’re taking St. John’s wort with SSRIs and calling it ‘wellness.’ This is just the tip of the iceberg. If you’re on any drug metabolized by CYP enzymes, you’re already at risk from a dozen other ‘natural’ products. Quercetin is just the latest scapegoat.
Chris Ashley
November 22, 2025 AT 16:38bro i took quercetin with my antidepressant for 8 months and felt like a god. now u saying it’s dangerous? i feel fine. maybe u just mad cause u don’t take supplements lol
Eleanora Keene
November 24, 2025 AT 04:10Thank you for sharing this. I’m a nurse and I’ve seen too many patients come in with unexplained side effects-only to find out they’re taking ‘just a little’ of something ‘natural.’ Please, if you’re reading this and you’re on meds: pause. Check. Talk to your pharmacist. You’re not being paranoid-you’re being smart.
kshitij pandey
November 24, 2025 AT 18:54From India, I’ve seen grandmas take turmeric and neem for everything. But they never take pills-they eat food. This article is so important. Supplements are not food. They’re concentrated. Please don’t treat them like vitamins. Talk to someone who knows your meds. Your life matters.
Nathan Hsu
November 26, 2025 AT 07:10Let me be clear: quercetin is not the enemy. The enemy is misinformation. The enemy is the supplement industry that markets 500mg pills as ‘immune boosters’ without a single warning. The FDA needs to act. Until then, educate yourself. Read the science. Don’t trust influencers. Trust peer-reviewed journals.