 Dec, 4 2025
Dec, 4 2025
When your skin breaks out in thick, scaly patches and your fingers or toes suddenly swell up like sausages, it’s not just bad luck-it’s your immune system sending a signal. Psoriatic arthritis isn’t just arthritis with a skin rash tacked on. It’s one condition, two faces: one on your skin, one in your joints. And if you’ve been told it’s just eczema or aging joints, you’re not alone. Nearly half of people with psoriatic arthritis wait over two years to get the right diagnosis. The good news? We know more now than ever about how the skin and joints are connected-and how to stop the damage before it’s too late.
How Skin and Joints Are Linked in Psoriatic Arthritis
Psoriatic arthritis happens because your immune system gets confused. It starts attacking your skin, causing those familiar red, flaky plaques. But then, it turns on your joints, tendons, and even the places where tendons attach to bone. This isn’t random. The same immune cells-T-cells and cytokines like TNF-alpha and IL-17-show up in both your psoriasis lesions and your inflamed joints. That’s why treating the skin often helps the joints, and vice versa.
Most people (about 85%) get skin psoriasis first. But here’s the twist: 15% of patients develop joint pain, stiffness, or swelling before any visible skin changes. That’s why doctors now check for nail changes-pitting, lifting, or crumbling-when someone comes in with unexplained joint pain. Nail problems are present in 80-90% of psoriatic arthritis cases, far more than in regular psoriasis alone. If you’ve got dented fingernails and a swollen knee, that’s not coincidence. It’s a red flag.
Key Signs You’re Not Just “Getting Older”
Not all joint pain is the same. Osteoarthritis wears down cartilage slowly. Rheumatoid arthritis hits both sides of the body symmetrically. Psoriatic arthritis? It plays by its own rules.
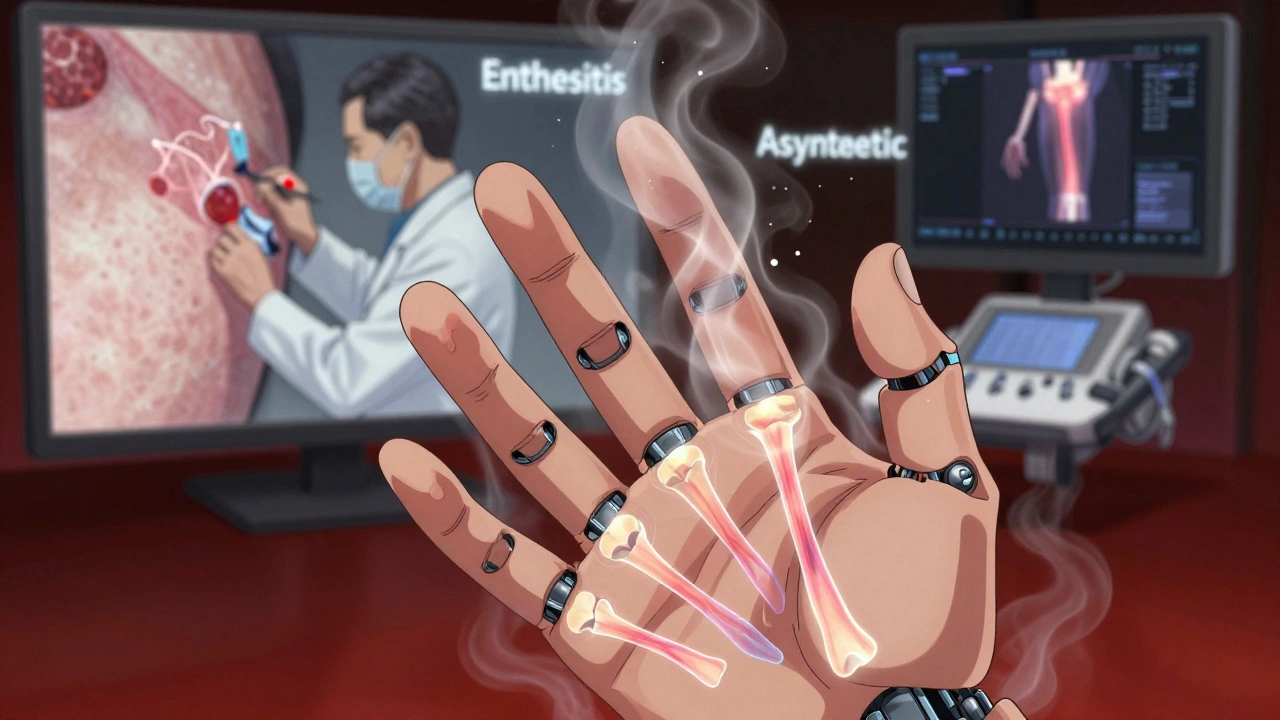
- Dactylitis: One or more fingers or toes swell up completely-like sausages. This happens in 40-50% of patients and is almost unique to psoriatic arthritis.
- Enthesitis: Pain where tendons meet bone. Think bottom of the foot (plantar fasciitis) or back of the heel (Achilles tendinitis). It’s not just soreness-it’s deep, sharp pain when you walk or stand.
- Asymmetric joint pain: Your right knee hurts, but your left one doesn’t. Your left wrist swells, but your right is fine. This pattern affects 70% of cases.
- Distal joint involvement: The joints closest to your nails (the ones you tap on your desk) are often the first to go. That’s different from rheumatoid arthritis, which hits knuckles first.
- Spinal stiffness: If your lower back or neck feels stiff in the morning and improves with movement, it could be spondylitis, a subtype affecting up to 20% of patients.
These signs don’t show up on regular X-rays early on. That’s why many people get misdiagnosed for years. Blood tests won’t help much either-90% of psoriatic arthritis patients test negative for rheumatoid factor, unlike those with rheumatoid arthritis. Diagnosis relies on clinical signs, skin history, and sometimes advanced imaging like ultrasound or MRI.
What the Experts Say About Early Treatment
Time is the enemy here. Dr. Laura Coates from the University of Oxford found that if you start treatment within 12 weeks of the first joint symptom, you prevent irreversible joint damage in 75% of cases. Left untreated, 30% of patients show major joint destruction within two years.
That’s why seeing both a rheumatologist and a dermatologist together is critical. About 45% of psoriatic arthritis cases are first spotted by dermatologists. If your skin doctor notices nail changes or joint swelling during a routine visit, they should refer you immediately. Waiting for the pain to get worse is a dangerous gamble.
Patients who delay treatment often end up needing stronger drugs later-or worse, joint replacements. One Reddit user, ‘PsOwarrior87,’ spent five years being treated for rheumatoid arthritis before switching to ustekinumab. Within three months, his joint swelling dropped by 80%. But he also had a scalp flare-up. That’s the trade-off: controlling one part of the disease can sometimes trigger another. That’s why treatment is personal.
Treatment Options: From Pills to Biologics
There’s no cure, but there are powerful tools to stop the damage. Treatment has evolved dramatically since the 2000s.
Traditional DMARDs like methotrexate are still used, especially in milder cases. They work slowly, over weeks or months, and can help reduce joint inflammation. But they don’t always touch skin symptoms well.
Biologics are the game-changers. These are injectable or IV drugs that block specific parts of the immune system-like TNF-alpha, IL-17, or IL-23. They work faster and are more targeted.
- TNF inhibitors (adalimumab, etanercept, infliximab): First-line biologics. About 55% of biologic prescriptions are for these. They help both skin and joints.
- IL-17 inhibitors (secukinumab, ixekizumab): Great for skin and dactylitis. Often used if TNF blockers don’t work.
- IL-23 inhibitors (guselkumab, risankizumab): Newer, with strong skin results. One user reported morning stiffness dropping from two hours to 20 minutes after switching to guselkumab.
- TYK2 inhibitor (deucravacitinib): First oral pill approved in 2022 for psoriatic arthritis. No injections. Works well for skin and joints, with fewer side effects than older oral drugs.
Oral JAK inhibitors like upadacitinib are coming soon, with results expected by late 2024. These could offer another pill option for those who hate needles.
But here’s the catch: biologics cost a lot. The average out-of-pocket cost is over $500 a month. Insurance approvals can take nearly two weeks. Many patients drop out because of cost or side effects-like injection site reactions (65%) or infections. That’s why treatment isn’t one-size-fits-all.
What You Can Do Right Now
You don’t have to wait for a specialist to take action.
- Track your symptoms. Keep a simple log: Which joints hurt? When? Did your skin change? Did you feel more tired? Apps or even a notebook help.
- Check your nails. Look for pits, ridges, or lifting. These are early warning signs.
- Ask for a referral. If you have psoriasis and joint pain, ask your dermatologist to refer you to a rheumatologist. Don’t wait for your GP to catch it.
- Start moving. Low-impact exercise like swimming, cycling, or yoga helps maintain joint flexibility. Physical therapy is often covered by insurance.
- Manage stress. Stress triggers flares. Meditation, breathing exercises, or even walking in nature can help.
Most patients need 3-6 months to learn their personal triggers. Fatigue is the hardest to manage-even when joints feel better, brain fog and exhaustion linger for 52% of people.
The Big Picture: Hope and Realism
Psoriatic arthritis used to mean disability. Today, with early treatment, most patients live full, active lives. Life expectancy is nearly normal. The risk of heart disease is higher-1.5 times the average-so managing blood pressure, cholesterol, and weight matters just as much as taking your meds.
AI is now predicting who’ll develop psoriatic arthritis from their psoriasis with 87% accuracy using nail and joint scans. By 2028, genetic testing may tell you which drug will work best for you-cutting out the trial-and-error that currently takes 2.3 treatments per patient.
This isn’t a death sentence. It’s a signal. Your body is telling you something’s off. Listen. Act fast. Treat both skin and joints together. And don’t let cost or confusion stop you from asking for help.
Can psoriatic arthritis develop without skin psoriasis?
Yes, but it’s uncommon. About 15% of people develop joint symptoms before any visible skin psoriasis appears. That’s why doctors look for nail changes, family history, and enthesitis when diagnosing. If you have unexplained joint pain and a close relative with psoriasis, you should still be evaluated for psoriatic arthritis-even without a rash.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis typically affects joints symmetrically (both hands, both knees) and shows up in blood tests as rheumatoid factor positive. Psoriatic arthritis is often asymmetric, affects tendons and nails, and is usually rheumatoid factor negative. It also causes dactylitis and enthesitis, which are rare in rheumatoid arthritis. The treatments overlap, but the underlying causes and patterns are different.
Do biologics cure psoriatic arthritis?
No, they don’t cure it. But they can put the disease into remission-meaning no active inflammation, no joint damage progression, and minimal symptoms. Many patients stay on biologics long-term because stopping them often leads to flare-ups. The goal isn’t to eliminate the disease forever, but to control it so it doesn’t control your life.
Why do some people get worse after starting treatment?
Some biologics, especially TNF inhibitors, can trigger new skin flares in a small number of people. Others may not respond well to the first drug tried. That’s why treatment is personalized. If one drug doesn’t work or causes side effects, switching to another-like an IL-23 or TYK2 inhibitor-is common and often successful. It’s not failure; it’s finding the right match.
Can diet or supplements help with psoriatic arthritis?
No diet or supplement can replace medication, but some people find that reducing sugar, processed foods, and alcohol helps with inflammation and fatigue. Omega-3 fatty acids from fish oil may offer mild benefit. Weight loss is one of the most effective non-drug strategies-every 10 pounds lost reduces joint stress and improves drug response. Always talk to your doctor before starting supplements, as some can interfere with biologics.
How often do you need blood tests while on biologics?
Before starting, you need screening for tuberculosis and hepatitis. After that, most patients get blood tests every 3-6 months to check liver function, blood counts, and infection markers. If you’re on methotrexate or JAK inhibitors, testing is more frequent. Your rheumatologist will tailor this based on your drug and health history.
Deborah Jacobs
December 5, 2025 AT 18:38My sister was misdiagnosed for three years with ‘just arthritis’-until she noticed her nails were crumbling. That’s when she pushed for a referral. Now she’s on secukinumab, and her dactylitis is gone. No more sausage fingers. It’s wild how something so small-nail changes-can be the key to unlocking the whole puzzle.
Don’t wait for the pain to be ‘bad enough.’ If you have psoriasis and even one weird joint symptom, go see a rheumatologist. Your future self will thank you.
Also, yoga. Do yoga. Even if you hate it. It’s the only thing that kept me walking when my knees felt like they were full of gravel.
Katie Allan
December 6, 2025 AT 17:50It’s not just about meds. It’s about listening to your body when it whispers before it screams. I used to ignore the stiffness in my knuckles because I thought I was just ‘getting old.’ Turns out, I was just getting sicker.
Tracking symptoms changed everything. I started writing down what I ate, how much I slept, and which joints hurt on which days. After two months, I saw a pattern: stress + sugar = flare. Not magic, just biology.
And yes, biologics are expensive-but so is losing your ability to hold your grandkid’s hand. I fought my insurance for six months. Won. Worth every email, every call, every tear.
sean whitfield
December 7, 2025 AT 03:38So let me get this straight. You’re telling me injecting expensive biologics into your arm is the modern miracle cure for… being alive? Wow. Next you’ll tell me sunlight causes cancer and we should all live in caves.
My grandpa had arthritis in the 50s. He walked with a cane. He didn’t have a smartphone app to track his ‘inflammation levels.’ He just lived. Maybe we’re overmedicalizing normal aging.
Also, ‘TYK2 inhibitor’? Sounds like a SpaceX rocket fuel.
Michael Dioso
December 9, 2025 AT 01:00Oh please. ‘Psoriatic arthritis isn’t just aging joints’-yeah, right. You’re telling me a 68-year-old with stiff knees and dry skin doesn’t have psoriatic arthritis? You’re just selling fear to sell drugs.
I’ve seen 12 different ‘specialists’ in my life. Every one of them had a new magic pill. None of them had a clue. The real cure? Stop stressing. Stop eating gluten. Stop believing in Big Pharma’s fairy tales.
And don’t even get me started on ‘biologics.’ You’re injecting lab-made antibodies like you’re in a sci-fi movie. What’s next? Nanobots?
Lucy Kavanagh
December 9, 2025 AT 05:59Did you know the WHO secretly classifies psoriatic arthritis as a ‘manufactured disease’ to push biologics? It’s all about profit. The nail changes? That’s just dehydration. The swelling? That’s from sitting too much at your desk job.
My cousin took ‘ustekinumab’ and developed a rash on her tongue. She’s now on a raw food diet and drinks distilled water. No more flares.
And why do dermatologists even refer you? They’re paid by pharma. Ask yourself: who funds the ‘research’? The same companies selling the $500/month shots.
Check your water supply. Check your EMF exposure. That’s the real trigger.
James Moore
December 10, 2025 AT 00:12Look, I’m an American, and I’ve seen this country turn everything into a medical crisis so corporations can profit-medical-industrial complex, baby. But here’s the thing: I’ve got a cousin in Germany who got his biologics covered by the state, and he still complains about the ‘injection anxiety.’
Meanwhile, in India, my friend Manish says they use turmeric paste and yoga-no pills, no shots, no insurance nightmares. And guess what? He walks fine.
So why are we in the U.S. paying $500 a month for something that other cultures treat with a spoonful of spice and a deep breath? It’s not science-it’s capitalism with a stethoscope.
And don’t get me started on ‘AI predicting disease.’ That’s just Big Brother with a lab coat. They’re not saving lives-they’re building databases. You think your genetic data is safe? It’s already sold three times.
Stop trusting doctors. Start trusting tradition. Stop injecting chemicals. Start eating like your ancestors did-before the FDA got involved.
Krishan Patel
December 10, 2025 AT 20:27It is a grave error to assume that modern pharmaceutical intervention is the only path to healing. In ancient Ayurvedic texts, psoriasis and joint afflictions were understood as manifestations of aggravated Vata and Kapha doshas, treated through panchakarma, dietary regulation, and herbal formulations such as neem, guggulu, and ashwagandha.
Modern medicine, with its reductionist approach, isolates cytokines and targets them with monoclonal antibodies, yet ignores the systemic imbalance that gave rise to the condition in the first place.
Furthermore, the obsession with biologics ignores the fact that 80% of chronic inflammatory conditions are modulated by gut microbiota, which is profoundly influenced by diet, sleep, and emotional stress-not by injecting proteins into the subcutaneous layer.
One must ask: is it healing, or merely suppression? And who benefits when the patient becomes dependent on a $60,000-per-year injection regimen?
True medicine restores balance. Not replaces function with a synthetic molecule.
Manish Shankar
December 12, 2025 AT 03:52I appreciate the detailed clinical overview presented in this post. As a medical professional from India, I have observed that many patients delay seeking rheumatology consultation due to socioeconomic barriers and lack of awareness.
It is commendable that the article emphasizes early referral and multidisciplinary care. In our setting, we often combine conventional therapy with patient education sessions led by trained nurses, which significantly improves adherence.
While biologics are transformative, their accessibility remains limited in low-resource regions. We have seen promising results with methotrexate combined with low-dose corticosteroids and physiotherapy, especially when initiated promptly.
Additionally, I would like to highlight the importance of mental health support. The psychological burden of chronic visible skin disease and persistent joint pain is often underestimated. Counseling should be integrated into routine care.
Thank you for raising awareness with evidence-based clarity.
Kylee Gregory
December 13, 2025 AT 01:28I think what’s missing from most of these conversations is the quiet, daily grief of living with a disease that nobody sees.
You get a flare and your hand swells up-you smile and say ‘oh, it’s nothing.’ You hide your nails. You wear long sleeves in summer. You don’t tell your boss why you can’t lift boxes. You don’t ask for help.
And then you read something like this and realize: I’m not broken. I’m not lazy. I’m not imagining it.
It’s not just about the meds. It’s about being seen.
Thank you for writing this. I wish I’d had it five years ago.
luke newton
December 14, 2025 AT 02:14You people are so desperate for a miracle cure you’ll swallow anything labeled ‘biologic’ and call it science. My cousin took that TYK2 pill and got shingles. Now he’s on steroids. Congrats, you traded one problem for two.
Meanwhile, I just take ibuprofen, stretch, and drink coffee. My joints are fine. Maybe the real problem isn’t your immune system-it’s your anxiety.
Stop buying into the fear. Stop spending $500 a month. Go for a walk. Breathe. You’ll be fine.
Also, ‘AI predicts arthritis’? Next they’ll say your soul is a data point.