 Oct, 3 2025
Oct, 3 2025
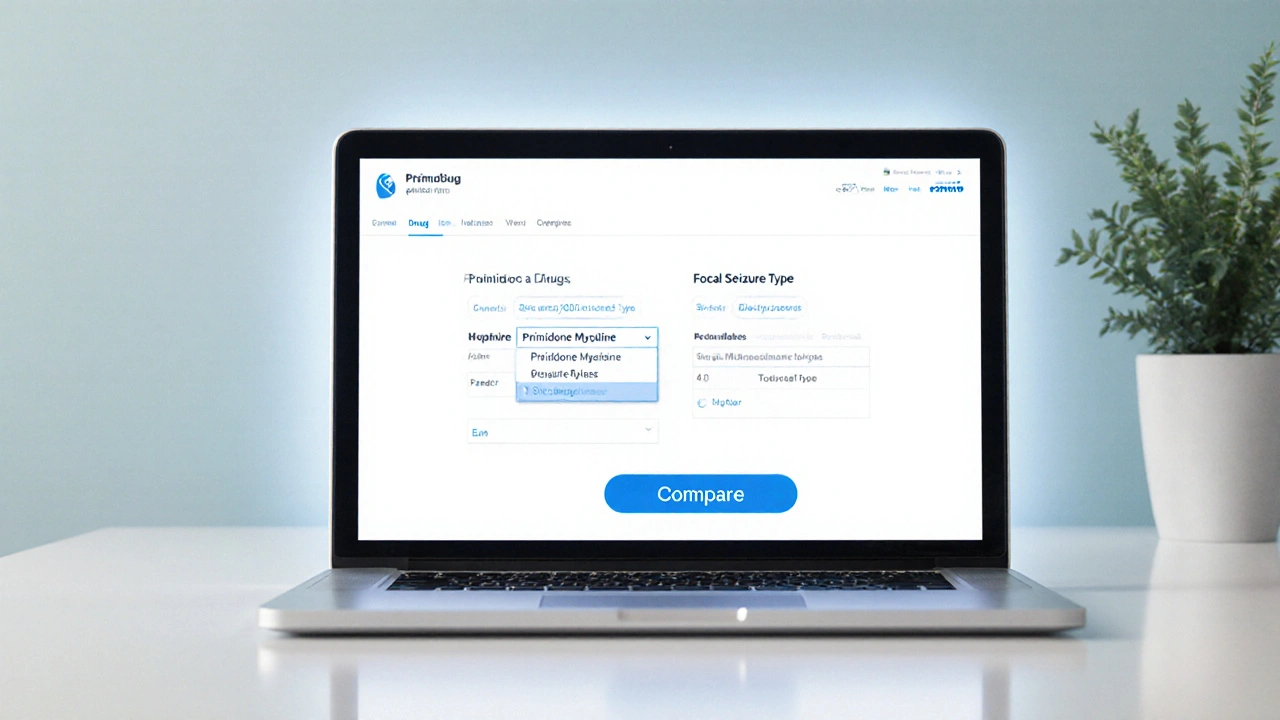
Anti-Seizure Drug Comparison Tool
Select a drug and seizure type, then click Compare to see detailed information.
If you or a loved one are facing epilepsy, the maze of medication choices can feel overwhelming. One name you’ll often see on prescriptions is Primidone (brand name Mysoline), a long‑standing option for focal and generalized seizures. But is it the right fit? Below we break down how Primidone stacks up against the most common alternatives, focusing on how they work, typical doses, side‑effect profiles, cost considerations, and when doctors might steer you toward one over another.
How Primidone Works and Who Typically Uses It
Primidone belongs to the barbiturate family. After ingestion, a portion is converted in the liver into phenobarbital, which then enhances the activity of the inhibitory neurotransmitter GABA. This dual action slows abnormal electrical spikes in the brain. It’s most often prescribed for:
- Essential tremor (off‑label but common)
- Partial (focal) seizures
- Generalized tonic‑clonic seizures
Typical starting doses for adults range from 50‑100mg daily, gradually titrated to 300‑600mg, depending on seizure control and tolerance.
Key Alternatives on the Market
Over the past two decades, newer agents have joined the anti‑seizure toolkit. Below are the most frequently considered alternatives to Primidone:
- Levetiracetam (brand Keppra): a pyrrolidine derivative that binds to synaptic vesicle protein 2A.
- Lamotrigine (brand Lamictal): blocks voltage‑gated sodium channels and reduces glutamate release.
- Carbamazepine (brand Tegretol): stabilises neuronal membranes by inhibiting repetitive firing.
- Phenytoin (brand Dilantin): another sodium‑channel blocker, but with a narrow therapeutic window.
- Valproic acid (brand Depakote): increases GABA levels and modulates ion channels.
- Phenobarbital: the classic barbiturate, still used in low‑resource settings.
Side‑Effect Profiles - What to Expect
Choosing a medication often comes down to how tolerable its side effects are for you. Here’s a quick snapshot:
| Drug | Common Mild Effects | Serious Risks |
|---|---|---|
| Primidone | Drowsiness, dizziness, nausea | Rare blood dyscrasias, severe skin reactions |
| Levetiracetam | Fatigue, irritability, loss of appetite | Psychiatric changes, rare rhabdomyolysis |
| Lamotrigine | Rash, headache, blurred vision | Stevens‑Johnson syndrome (very rare) |
| Carbamazepine | Blurred vision, nausea, hyponatremia | Aplastic anemia, severe skin reactions |
| Phenytoin | Gum overgrowth, tremor, hirsutism | Cardiotoxicity, severe liver injury |
| Valproic acid | Weight gain, tremor, hair loss | Liver failure, pancreatitis, teratogenicity |
| Phenobarbital | Sleepiness, constipation | Dependence, respiratory depression |
Notice how Primidone’s most frequent complaints are sedation and nausea - a pattern familiar with barbiturates. Newer drugs like Levetiracetam tend to cause mood‑related issues, while Lamotrigine’s hallmark risk is a severe rash that requires immediate medical attention.

Effectiveness Across Seizure Types
Clinical trials and real‑world data give us a sense of how well each drug controls seizures:
- Primidone: solid efficacy for focal seizures; works well when combined with other agents.
- Levetiracetam: broad spectrum - effective for focal, generalized, and myoclonic seizures; often first‑line for adults.
- Lamotrigine: excellent for focal seizures and for preventing secondary generalisation; also used in bipolar disorder.
- Carbamazepine: gold standard for focal seizures but can worsen certain generalized types.
- Phenytoin: historically first‑line for tonic‑clonic seizures; now reserved for refractory cases.
- Valproic acid: the most versatile - covers focal, generalized, and absence seizures, but not ideal for women of childbearing age.
- Phenobarbital: reliable for many seizure types but limited by sedation and dependence.
When doctors pick a drug, they weigh seizure type, patient age, comorbidities, and lifestyle. For a young adult with focal seizures and no liver issues, Levetiracetam or Lamotrigine often supersede Primidone because they’re easier on the mind.
Cost and Availability in the UK (2025)
Affordability matters, especially with long‑term therapy. Below is a rough price range for a typical monthly supply (based on NHS prescription data for 2025):
- Primidone (Mysoline): £5‑£8
- Levetiracetam (Keppra): £12‑£20
- Lamotrigine (Lamictal): £8‑£15
- Carbamazepine (Tegretol): £6‑£10
- Phenytoin (Dilantin): £4‑£7
- Valproic acid (Depakote): £9‑£16
- Phenobarbital: £3‑£5
Primidone remains one of the cheapest options, which explains its continued use in primary‑care settings. However, price alone shouldn’t dictate choice if side effects compromise quality of life.
When Doctors Prefer One Drug Over Another - Decision‑Making Guide
Here’s a quick decision tree you can discuss with your neurologist:
- If you’re a woman of child‑bearing potential, avoid Valproic acid and consider Lamotrigine or Levetiracetam.
- For patients with a history of severe skin reactions, steer clear of Carbamazepine and Lamotrigine.
- If you need rapid seizure control and can tolerate sedation, Primidone or Phenobarbital are viable.
- When mood changes are a concern, Levetiracetam may require close monitoring; Lamotrigine is mood‑stabilising.
- Kidney or liver impairment: dose‑adjust Phenytoin and Valproic acid accordingly, or choose Primidone (which has a predictable metabolism).
Every patient’s story is unique, so a trial period of 4-8 weeks with careful monitoring is typical before confirming the optimal drug.
Practical Tips for Switching From Primidone to Another Medication
Changing anti‑seizure meds can be tricky. Follow these steps to reduce break‑through seizures:
- Consult your neurologist before any alteration - they’ll outline a taper schedule.
- Gradually reduce Primidone by 25mg every 3‑5 days while introducing the new drug at a low dose.
- Track seizure frequency and side‑effects in a daily journal.
- Arrange a blood test if the new drug requires therapeutic drug monitoring (e.g., Phenytoin, Valproic acid).
- Maintain a consistent sleep schedule and avoid alcohol, as both can destabilise seizure control during the transition.
Most patients notice a steady improvement within a month, but some may need a second medication to fill gaps.

Frequently Asked Questions
What makes Primidone different from newer anti‑seizure drugs?
Primidone is a barbiturate that converts partly into phenobarbital, giving it a double‑action mechanism. Newer drugs like Levetiracetam work on synaptic proteins, usually causing fewer cognitive side effects. Primidone’s advantage is low cost and a well‑known safety profile, but sedation is more common.
Can I take Primidone with other anti‑seizure medications?
Yes, it’s often combined with drugs like Levetiracetam or Lamotrigine to boost efficacy while keeping each dose low. Always check with your doctor because Primidone can increase the levels of certain enzymes, affecting the metabolism of other meds.
Is Primidone safe for long‑term use?
Long‑term use is generally safe if you tolerate it well. Periodic blood tests are advised to monitor liver function and blood counts, especially after the first year of therapy.
How quickly does Primidone start working?
Because it’s partially converted to phenobarbital, you may notice seizure reduction within 1‑2 weeks, but full effect can take 4‑6 weeks of steady dosing.
What are the most common reasons doctors switch patients off Primidone?
Intolerable drowsiness, cognitive fog, or significant nausea are the top complaints. If the seizure frequency remains high despite maximal doses, a newer drug with a broader spectrum may be tried.
Samson Tobias
October 3, 2025 AT 20:33Thanks for pulling together such a thorough comparison; it really helps anyone sifting through the options. I appreciate the clear breakdown of mechanisms and side‑effect profiles. The cost table is especially handy for patients on a tight budget. It’s also good to see the practical switching tips – they’re often missing from the literature. Keep up the solid work!
Alan Larkin
October 10, 2025 AT 20:33Honestly, you could have cut the fluff and just shown the pharmacokinetic numbers straight away. Everyone already knows barbiturates are sedating, no need to repeat it. Also, why not include the enzyme‑inducing potential of carbamazepine? It matters for drug‑drug interactions. :)
John Chapman
October 17, 2025 AT 20:33While the article is serviceable, it fails to acknowledge the nuanced role of GABA‑ergic modulation in refractory epilepsy, a topic extensively covered in the latest neuropharmacology treatises. Moreover, the omission of recent meta‑analyses on levetiracetam’s cognitive profile is a glaring oversight. One expects a higher scholarly standard.
Tiarna Mitchell-Heath
October 24, 2025 AT 20:33Stop beating around the bush – primidone is outdated and you should just prescribe levetiracetam. The sedation alone makes it unacceptable for any active adult.
Katie Jenkins
October 31, 2025 AT 19:33Actually, the “fluff” you refer to serves a purpose for patients who aren’t versed in pharmacology. While enzyme induction is indeed critical, the article does list carbamazepine’s effect on hepatic enzymes in the side‑effect table. For completeness, adding a brief note on CYP3A4 interaction could satisfy both clinicians and lay readers alike. The balance between depth and accessibility is always a tricky dance, but this piece leans more toward the latter, which is appropriate for a general audience. The balance between depth and accessibility is always a tricky dance, but this piece leans more toward the latter, which is appropriate for a general audience. :)
Jack Marsh
November 7, 2025 AT 19:33One could argue that the cost comparison undervalues the hidden expenses of monitoring serum levels for drugs like phenytoin and valproic acid. These ancillary costs can offset the apparent savings of cheaper agents such as primidone.
Terry Lim
November 14, 2025 AT 19:33That's exactly why many neurologists simply avoid those older drugs.
Cayla Orahood
November 21, 2025 AT 19:33What the mainstream medical literature refuses to tell you is that the very existence of a cheap, “legacy” drug like primidone is no accident. Behind the scenes, pharmaceutical conglomerates have been subsidizing its production to keep a foothold in markets that cannot afford the newer, patent‑protected options. This creates an illusion of choice while cementing dependency on a drug whose side‑effect profile is deliberately downplayed. The sedation you experience is not merely a pharmacological effect; it is a subtle tool to reduce patient alertness and compliance. When patients are drowsy, they are less likely to question dosing schedules or demand alternative therapies. Meanwhile, the newer entrants, such as levetiracetam, are marketed with glossy campaigns that obscure their own long‑term metabolic footprints. The cost‑saving narrative also masks the hidden price of reduced productivity and quality of life. Moreover, the regulatory agencies have been slow to update guidelines, allowing older drugs to persist in formularies long after better options have emerged. This inertia benefits a network of prescribers who have been trained on these agents during residency, creating a cycle of habit over evidence. In addition, the patent for phenobarbital, the active metabolite of primidone, has expired for decades, ensuring a steady, low‑margin profit stream for generic manufacturers. Such manufacturers often lobby to keep the drug on essential medicines lists, arguing that “affordability” outweighs the drawbacks. Yet affordability should never be a euphemism for compromising neurological health. The subtle risk of rare blood dyscrasias, silently noted in the side‑effect table, has been linked in obscure case studies to immune dysregulation that can persist long after drug cessation. This is the kind of detail that never makes the headline but matters profoundly for patient safety. Ultimately, the decision to stay on primidone may reflect more than clinical efficacy; it may reflect an entrenched system that prioritizes profit and convenience over genuine therapeutic advancement.
McKenna Baldock
November 28, 2025 AT 19:33I see where you're coming from, and it's true that cost considerations often drive prescribing habits. However, I think it's also worth noting that many patients truly benefit from primidone's predictable pharmacokinetics. The simplicity of dosing can be a tangible advantage, especially for those with limited healthcare access. Still, a balanced discussion that acknowledges both the economic and safety dimensions would serve the community best.
Roger Wing
December 5, 2025 AT 19:33People love to brag about “new” drugs but forget the old ones had years of real world data they just toss away like yesterday's news the side effects are well documented and the price is unbeatable
Matt Cress
December 12, 2025 AT 19:33Sure, because the best medical practice is to base decisions solely on price tags and ignore any advances in safety. Who needs research when you have nostalgia?
Andy Williams
December 19, 2025 AT 19:33The data speak for themselves.
Paige Crippen
December 26, 2025 AT 19:33They don’t want you to see the hidden safety reports.
sweta siddu
January 2, 2026 AT 19:33Great job summarizing everything, really helpful! 😊👍