 Jan, 16 2026
Jan, 16 2026
Medication Photosensitivity Checker
Check if your medications might increase your sun sensitivity. This tool identifies photosensitivity risk based on common medications and provides tailored protection advice.
How This Works
This tool identifies medications that commonly cause photosensitivity. Results are based on clinical evidence from the article, but always consult your doctor for personalized advice.
Important: Medication photosensitivity is not guaranteed for everyone. This tool provides general information only.
What Is Medication-Induced Photosensitivity?
You take your pill like clockwork, but then you step outside for five minutes and your skin turns bright red, burns, or peels like you’ve been at the beach all day. If this sounds familiar, you might be dealing with photosensitivity from your medication. It’s not just a bad sunburn-it’s your body reacting to sunlight because of something you’re taking. About 1,000 common medications can cause this, and up to 20% of people on these drugs will experience it. Many don’t even know it’s possible until they get burned.
There are two main types: phototoxic and photoallergic reactions. Phototoxic is the most common-about 95% of cases. It happens fast. Within minutes to a couple of hours after sun exposure, your skin gets red, swollen, and painful, just like a bad sunburn but worse. It usually stays only where the sun hit. Photoallergic is rarer, but sneakier. It can show up a day or two later as an itchy, spreading rash that looks like eczema, even on skin covered by clothes. This one’s an immune response, not just chemical damage.
Which Medications Cause Sun Sensitivity?
Some of the most common culprits are things you’d never expect to burn you. Antibiotics like doxycycline and ciprofloxacin are big ones. If you’re on doxycycline for acne or an infection, 10-20% of people will get phototoxic burns-even through light clothing. NSAIDs like ketoprofen (found in some topical pain gels) can do the same. Even some heart meds, like amiodarone, cause long-term sensitivity. People on it for years can still burn decades after stopping.
Other offenders include diuretics, some antidepressants, and even certain acne treatments like isotretinoin. And don’t forget sunscreen ingredients-oxybenzone, which is in many sunscreens, can actually cause photoallergic reactions in some people. That’s right: your sunscreen might be making it worse.
Women are more likely to get photoallergic reactions, mostly because they use more topical products-creams, lotions, makeup-that contain these sensitizing chemicals. If you’re on any of these meds and live in a place with bright sun-even in winter-you need to treat your skin like it’s fragile.
Why Regular Sunscreen Isn’t Enough
Most people think SPF 30 is enough. It’s not. For medication-induced photosensitivity, you need SPF 50+ with high UVA protection. Why? Because the damage comes mostly from UVA rays, not UVB. UVB causes sunburns. UVA penetrates deeper, passes through glass and clouds, and triggers the chemical reactions in your skin that lead to burns and long-term damage.
Here’s the problem: many SPF 50 sunscreens still don’t block enough UVA. The FDA says only 35% of high-SPF sunscreens meet the UVA protection standard. Look for ingredients like zinc oxide or titanium dioxide-they physically block both UVA and UVB. Avoid chemical filters like avobenzone unless they’re stabilized with other ingredients. And don’t rely on the number alone. A product labeled “broad spectrum” doesn’t always mean it’s strong enough.
Apply at least one ounce-about a shot glass full-for your whole body. Most people use only a quarter of that. That means you’re getting half the protection you think you are. Reapply every two hours, or after sweating or wiping your skin. If you’re on a high-risk medication, treat sunscreen like medicine: non-negotiable, every single day.

Physical Barriers Work Better Than You Think
Here’s what actually works: clothing that blocks UV. Standard cotton t-shirts only block about 5% of UV rays when wet. A regular denim shirt? Maybe 20%. But UPF 50+ clothing blocks 98%. That’s not marketing-it’s lab-tested fact.
Brands like Solbari, Coolibar, and UV Skinz make shirts, hats, and even gloves designed for people with photosensitivity. One user on MyHealthTeams said switching to UPF 50+ clothing cut their reactions by 90%. No more burning during a quick walk to the mailbox. No more hiding indoors in spring. And it’s not just for beach days. These clothes are lightweight, breathable, and look like regular clothes.
Wear wide-brimmed hats, UV-blocking sunglasses, and consider window films if you sit near a sunny window at home or in the car. UVA penetrates glass. You can get burned driving to work.
How to Know If You’re at Risk
If you’ve ever had an unexplained sunburn after starting a new medication, that’s a red flag. But many doctors don’t warn patients. A 2022 survey found that 68% of people with medication-induced photosensitivity were never told about the risk when they got their prescription.
Ask yourself: Did your skin change after starting a new drug? Did the burn happen faster or worse than usual? Did it spread beyond sun-exposed areas? If yes, talk to your doctor. Bring a list of every medication, supplement, and topical product you use.
There’s a test called photopatch testing that can confirm photoallergy, but it’s only done in specialty clinics and only works in 30-40% of cases. Most of the time, diagnosis comes from your history-what you took, when you got burned, and how it looked.
What to Do If You Get a Reaction
If you get a phototoxic burn: get out of the sun immediately. Cool the skin with damp cloths. Use aloe vera or hydrocortisone cream (1%) to reduce inflammation. Avoid popping blisters. Take ibuprofen for pain and swelling. If it’s severe-blisters covering a large area, fever, or signs of infection-go to urgent care.
For photoallergic rashes: stop the suspected medication only if your doctor says so. Don’t quit cold turkey. These rashes can last weeks. Antihistamines help with itching. Topical steroids may be needed. Avoid scratching. The rash can spread even if you’re no longer in the sun.
Keep a symptom diary. Note the date, what you took, how long you were outside, the weather, and how your skin reacted. This helps your doctor spot patterns.
New Tools and Future Solutions
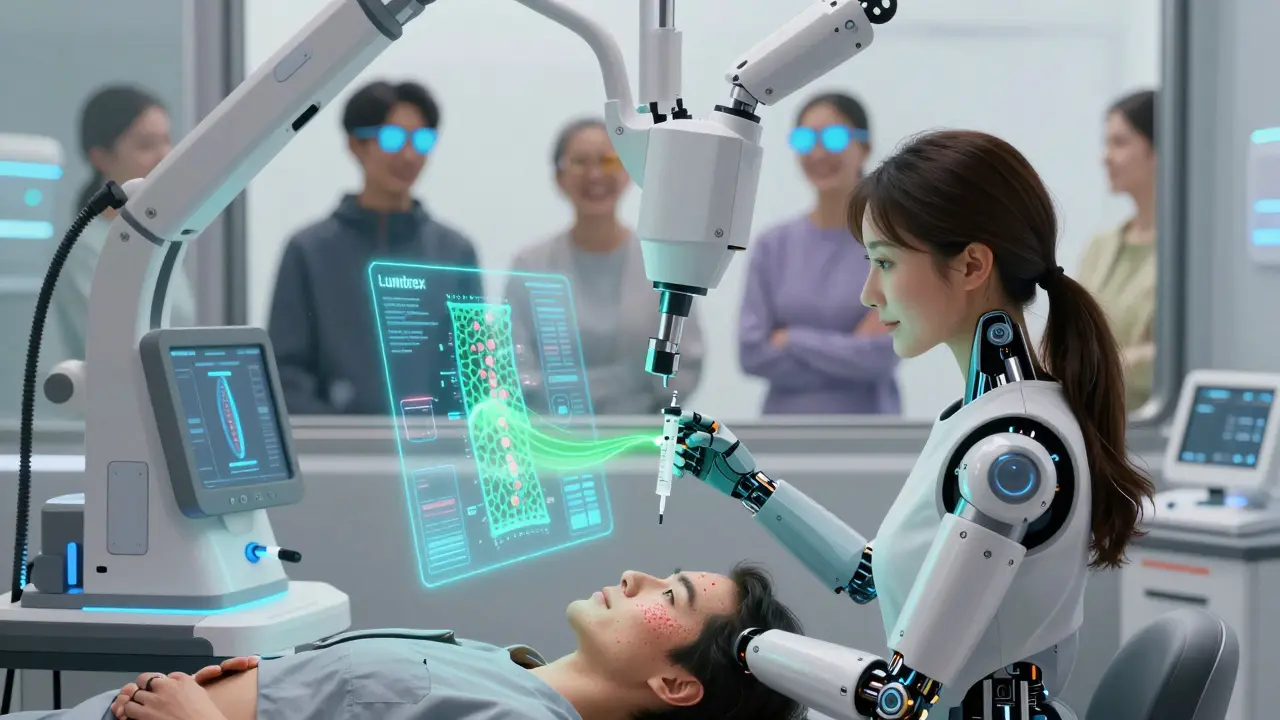
Things are changing. In 2023, the FDA approved the first drug specifically designed to reduce UV damage from medications: Lumitrex. It works by blocking reactive oxygen species-the chemicals that burn your skin. Early results show it cuts damage by 70%.
Meanwhile, companies are developing “smart” sunscreens that change color when UV levels get dangerous. Some apps, like UVLens, give real-time UV index alerts and tell you how long you can safely stay out based on your meds and skin type.
Even more promising: genetic testing. 23andMe now offers a photosensitivity risk panel that checks for gene variants linked to higher reaction risk. If you have a family history of sun sensitivity or skin cancer, it’s worth considering.
What You Can Do Today
- Check every medication you take for photosensitivity warnings. Look up your drugs on the FDA’s Sun Safety Medication Database.
- Switch to SPF 50+ mineral sunscreen with zinc oxide or titanium dioxide as the first two ingredients.
- Buy at least one UPF 50+ item-hat, shirt, or arm sleeves-and wear it daily.
- Check the UV index every morning. If it’s above 3, take extra precautions.
- Never assume you’re safe on cloudy days or in winter. UVA is always there.
- Talk to your pharmacist or dermatologist. Ask: “Is this medication known to cause sun sensitivity?”
Photosensitivity isn’t just an annoyance. It raises your risk of skin cancer by up to 60% over time. The good news? You can control it. It’s not about avoiding the sun forever-it’s about protecting yourself smartly. With the right tools, you can live normally without fear of burning.
Can I still go outside if I’m on a photosensitizing medication?
Yes, but you need to be smart. Limit direct sun exposure during peak hours (10 a.m. to 4 p.m.), wear UPF 50+ clothing, use SPF 50+ mineral sunscreen, and check the UV index daily. You don’t have to stay indoors-just protect yourself like you would in a high-risk environment.
Does sunscreen block all UV rays from triggering a reaction?
No. Most sunscreens don’t block enough UVA, which is the main trigger. Even SPF 50 sunscreens with only chemical filters may leave you vulnerable. Zinc oxide and titanium dioxide offer the most reliable protection. For maximum safety, combine sunscreen with physical barriers like clothing and shade.
How long does photosensitivity last after stopping the medication?
It varies. For most drugs, sensitivity fades within days to weeks after stopping. But some, like amiodarone, can cause reactions for up to 20 years. If you were on a long-term medication, assume you’re still at risk unless your doctor says otherwise.
Can I use tanning beds if I’m photosensitive?
Absolutely not. Tanning beds emit intense UVA radiation-often stronger than the midday sun. If your skin reacts to sunlight from medication, tanning beds can cause severe burns, blistering, and long-term skin damage. Avoid them completely.
Are children at risk for medication-induced photosensitivity?
Yes. Children on antibiotics like doxycycline (used for Lyme disease or acne) or isotretinoin for severe acne can develop phototoxic reactions. Always check medication labels and ask the prescribing doctor about sun safety. Kids’ skin is more sensitive, so protection is even more critical.
Should I get genetic testing for photosensitivity risk?
If you’ve had repeated unexplained sun reactions, or have a family history of skin cancer or autoimmune conditions, yes. The 23andMe photosensitivity panel checks genes linked to higher risk, like MC1R. It’s not necessary for everyone, but it can help personalize your protection strategy.
Cheryl Griffith
January 16, 2026 AT 18:36I didn't realize how many common meds cause this until I read this. I was on doxycycline for acne and thought I was just getting a bad sunburn every spring. Turned out I was burning through my shirt. Now I wear UPF 50+ tees year-round. Game changer.
Corey Sawchuk
January 18, 2026 AT 07:16My dermatologist never mentioned this when I got my amiodarone prescription. I’ve been burned twice since starting it. Guess I’m learning the hard way. Thanks for the heads up.
evelyn wellding
January 20, 2026 AT 00:05UPF clothing is literally life-changing 😍 I got a hat and arm sleeves and now I can actually go for walks without panicking. Also the UVLens app is legit.
Ryan Hutchison
January 20, 2026 AT 06:33Stop being so weak. If you can’t handle the sun, don’t take the meds. America’s gotten too soft. People in other countries deal with this daily and don’t whine about it. Just wear a shirt and stop acting like you’re in a lab experiment.
Nicholas Gabriel
January 21, 2026 AT 13:18As someone who’s been managing photosensitivity for over a decade-yes, it’s real, yes, it’s underdiagnosed, and yes, sunscreen alone is useless. I’ve used zinc oxide-based sunscreens since 2018, and I swear by them. Also, don’t forget: window film on your car and home windows cuts UVA exposure by 90%. I didn’t know this until I got burned driving to work in December. The sun doesn’t care if it’s cold. It doesn’t care if you’re inside. UVA penetrates everything.
And yes, your sunscreen can cause the reaction. I had a photoallergic rash from oxybenzone-so I switched to non-nano zinc oxide, and it stopped overnight. People think ‘broad spectrum’ means ‘safe.’ It doesn’t. Look at the ingredients. If zinc or titanium dioxide aren’t the first two, it’s not enough. Also, reapplying every two hours isn’t optional-it’s medical necessity. I’ve seen people burn through SPF 100 because they used a teaspoon on their whole body. That’s not sunscreen. That’s a joke.
And if you’re on amiodarone? You’re probably still photosensitive. Even if you stopped it five years ago. The drug lingers in fat tissue. I know someone who burned after stopping it 17 years prior. So don’t assume you’re in the clear. Talk to a dermatologist who actually knows this stuff. Most general practitioners don’t. I had to find one through a photosensitivity support group.
And yes, tanning beds are a death trap. They’re like a UV flamethrower. And no, children aren’t immune. My nephew got burned on doxycycline for Lyme disease at age 11. He still has scars. So if you’re a parent-ask the doctor. Don’t wait for the burn to happen.
Genetic testing? If you’ve got red hair, freckles, or a family history of melanoma-it’s worth it. MC1R variants are a huge risk factor. 23andMe’s panel isn’t perfect, but it’s better than guessing. I got mine done. It confirmed what I already suspected. And now I treat every day like it’s a 10 on the UV index. Because it might as well be.
And if you’re thinking, ‘I’m fine, I don’t burn’-you’re lying to yourself. You might not burn visibly, but you’re still accumulating DNA damage. That’s how skin cancer sneaks up on you. This isn’t about vanity. It’s about survival.
Melodie Lesesne
January 22, 2026 AT 06:29This is so helpful! I just started a new antidepressant and noticed my arms got red after walking the dog. Thought it was just allergies. Now I’m checking the med list and buying a UPF shirt. Thanks for making it so clear.
john Mccoskey
January 22, 2026 AT 20:57Let me break this down for the emotionally overwhelmed. You are not special. You are not fragile. You are taking a pharmaceutical compound that alters your biochemistry. That compound interacts with ultraviolet photons. That interaction triggers a photoreaction. This is not a conspiracy. This is not a marketing ploy by Coolibar. This is physics and pharmacology. You are a chemical system. Sunlight is energy. Your skin is a receptor. When the energy hits the wrong molecule, it causes oxidative stress. That is not a bug. That is a feature of the molecule’s structure. You are not being punished. You are being informed. The solution is not to avoid the sun. The solution is to understand the mechanism. Zinc oxide is a physical barrier. It reflects photons. It does not absorb them. That is why it works. Avobenzone absorbs photons and degrades. That is why it fails. You are not a victim. You are a data point. Your skin is a sensor. Learn to read it. Stop treating your body like a temple. Treat it like a laboratory. And stop buying into the wellness industrial complex. UPF clothing is not a lifestyle brand. It is a functional tool. Like a seatbelt. Like a helmet. Use it. Or don’t. But don’t pretend ignorance is a virtue.
Bianca Leonhardt
January 22, 2026 AT 22:30People who don’t read the medication leaflets deserve to get burned. If you didn’t look up the side effects, you’re not a victim-you’re negligent. And don’t blame the doctor. You signed the consent form. You had access to the internet. You chose to ignore it. Now you’re crying about it? Grow up.
Corey Chrisinger
January 24, 2026 AT 14:50It’s wild how we’ve turned sun exposure into this moral dilemma. We’re told to avoid the sun like it’s evil, but we also get told to get vitamin D. We’re told to wear sunscreen, but then told sunscreen might be toxic. We’re told to use UPF clothing, but then told it’s ‘performative.’ What’s the truth? The truth is we’re all just trying to survive in a world that’s changing faster than our biology can adapt. The sun isn’t the enemy. The system is. We’re given drugs without context. We’re sold sunscreens without transparency. We’re told to protect ourselves, but nobody tells us how to actually do it. So we’re left confused, burned, and guilty. Maybe the real solution isn’t more gear or more apps. Maybe it’s asking why we’re being put in this position in the first place.