 Jan, 1 2026
Jan, 1 2026
What Is CKD-Mineral and Bone Disorder?
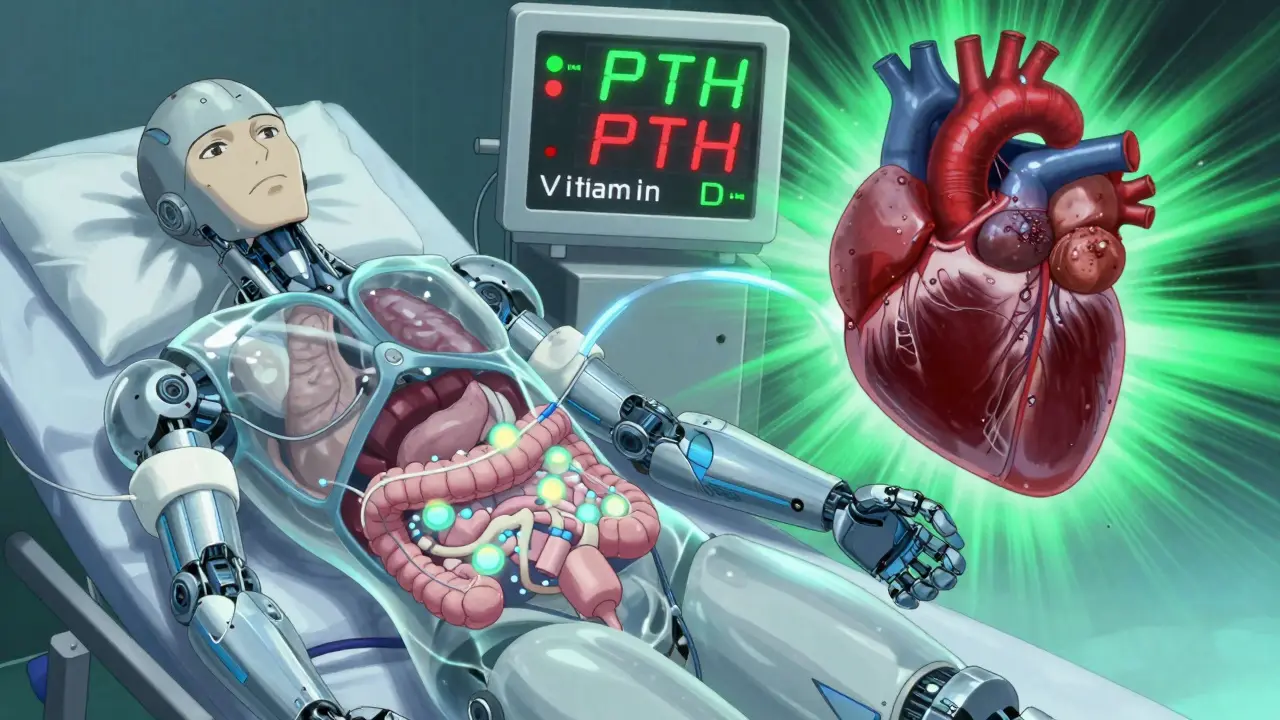
When your kidneys start to fail, they don’t just stop filtering waste-they also lose their ability to keep your bones and blood chemistry in balance. This isn’t just about weak bones. It’s a systemic problem called CKD-Mineral and Bone Disorder (CKD-MBD), a complex web of imbalances involving calcium, phosphate, parathyroid hormone (PTH), and vitamin D. It affects nearly everyone with advanced kidney disease, and it’s one of the leading reasons people with chronic kidney disease (CKD) die-not from kidney failure itself, but from heart attacks and broken bones.
The Three-Part Problem: Calcium, PTH, and Vitamin D
Think of CKD-MBD as a broken feedback loop. When kidney function drops below 60 mL/min (Stage 3 CKD), three things start going wrong at once:
- Phosphate builds up because the kidneys can’t flush it out.
- Vitamin D stops being activated, so your body can’t absorb calcium from food.
- Your parathyroid glands go into overdrive, pumping out too much PTH to try and fix the calcium shortage.
This isn’t a case of one thing causing another-it’s a cycle. High phosphate triggers high PTH. Low vitamin D makes calcium drop. High PTH then pulls calcium out of your bones, making them brittle. Meanwhile, calcium and phosphate start sticking to your blood vessels, turning them stiff and prone to rupture.
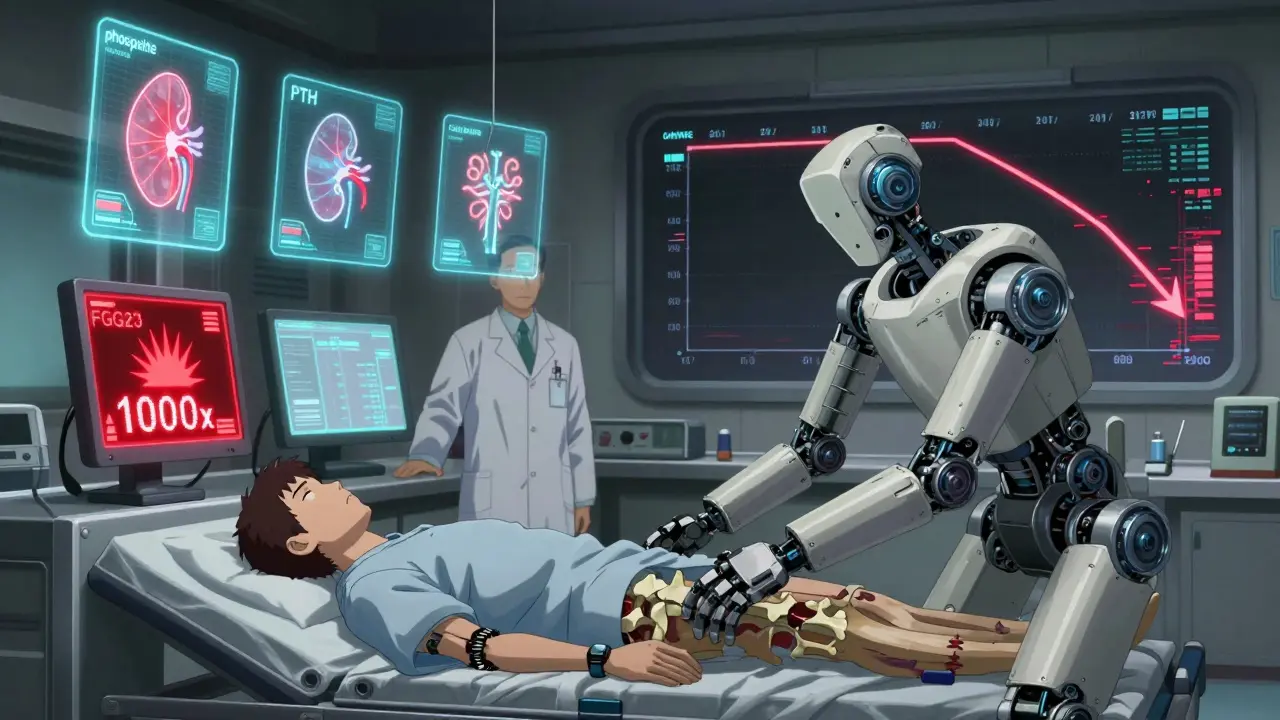
Why Phosphate Is the Silent Driver
Most people focus on calcium and vitamin D, but phosphate is the real engine behind CKD-MBD. In healthy people, kidneys remove excess phosphate daily. In CKD, that system breaks down. By Stage 4, phosphate levels are already rising. By Stage 5 (dialysis), over 70% of patients have phosphate above 4.5 mg/dL-the upper limit of normal.
When phosphate climbs, your bones release a hormone called FGF23 to tell the kidneys to excrete more. But in CKD, the kidneys can’t respond. So FGF23 keeps rising-sometimes 1000 times higher than normal. That’s when things get dangerous. High FGF23 suppresses the active form of vitamin D, worsens calcium deficiency, and directly damages the heart muscle. Studies show every 1 mg/dL increase in phosphate raises your risk of death by 18%.
Vitamin D: Not Just for Bones
You’ve heard vitamin D is for bones. In CKD, it’s more than that. Your kidneys convert vitamin D from food or sun exposure into its active form, calcitriol. When kidneys fail, that conversion drops by 50-80%. That means even if you take vitamin D supplements, your body can’t use them properly.
Eighty to ninety percent of people with Stage 3-5 CKD are vitamin D deficient. That’s not just a lab number-it’s linked to a 30% higher risk of dying. But here’s the twist: giving active vitamin D (like calcitriol) can backfire. It raises calcium and phosphate levels, which can speed up artery calcification. That’s why most guidelines now recommend starting with regular vitamin D (cholecalciferol), not the active form, unless PTH is sky-high. A 2023 study found that regular vitamin D cuts mortality risk by 15% without the side effects.
PTH: Too High or Too Low-Either Way, It’s Bad
Parathyroid hormone (PTH) is your body’s emergency response to low calcium. In early CKD, PTH rises to pull calcium from bones. That’s normal compensation. But over time, the parathyroid glands grow too big and become independent. They keep pumping out PTH even when calcium is normal-or even high.
But here’s what most people don’t realize: low PTH can be just as dangerous. About half of dialysis patients have something called adynamic bone disease-where PTH is too low (under 150 pg/mL). Their bones stop remodeling. They don’t break down old bone or build new bone. The result? Bones that look normal on a scan but are fragile and prone to fractures. This is why doctors don’t just aim for "normal" PTH-they aim for a range: 2 to 9 times the upper limit of your lab’s normal value. Too high? Bone loss. Too low? Silent bone failure.
Calcium: The Tightrope Walk
Calcium levels in CKD patients are a balancing act. You want to avoid low calcium because it triggers PTH spikes. But you also don’t want high calcium because it teams up with phosphate to calcify your heart and arteries.
Most guidelines recommend keeping serum calcium between 8.4 and 10.2 mg/dL. But getting there is tricky. Calcium-based phosphate binders (like calcium acetate) help lower phosphate-but each pill adds more calcium to your system. That’s why doctors limit calcium-based binders to 1500 mg of elemental calcium per day. Too much? You’re feeding vascular calcification.
That’s why non-calcium binders like sevelamer or lanthanum are often preferred. They lower phosphate without adding calcium. But they’re more expensive. For many patients, the choice comes down to cost versus long-term heart risk.
What Does This Look Like in Real Life?
Meet a 62-year-old man on dialysis for 3 years. His labs show:
- Phosphate: 6.1 mg/dL
- PTH: 850 pg/mL
- Calcium: 9.8 mg/dL
- 25(OH)D: 18 ng/mL
He’s got high phosphate, very high PTH, and low vitamin D. His bones are being eaten away. His arteries are hardening. He’s at 5 times higher risk of a heart attack than someone his age without kidney disease.
His treatment? A low-phosphate diet (no soda, processed cheese, or instant meals), sevelamer with meals, 2000 IU of vitamin D daily, and cinacalcet to lower PTH. Within 6 months, his phosphate drops to 5.0, PTH to 450, and vitamin D to 32. His fracture risk goes down. His heart doesn’t calcify as fast. He’s not cured-but he’s buying time.
How Is It Diagnosed?
You won’t feel CKD-MBD until it’s advanced. No pain. No swelling. Just a slow decline. That’s why labs are everything.
Doctors check four things every 3-6 months in Stage 3-5 CKD:
- Serum phosphate (target: 2.7-4.6 mg/dL for early CKD; 3.5-5.5 for dialysis)
- Serum calcium (target: 8.4-10.2 mg/dL)
- Intact PTH (target: 2-9x upper normal limit)
- 25-hydroxyvitamin D (target: at least 30 ng/mL)
Bone biopsies are the gold standard to see if bone turnover is high, low, or normal-but they’re invasive. Fewer than 5% of patients get them. Instead, doctors use blood markers like bone-specific alkaline phosphatase (BSAP) and PINP to guess what’s happening inside the bone.
For blood vessels, a simple chest X-ray can show calcification in the heart arteries. But CT scans give the real picture. By Stage 5, 80% of dialysis patients have visible coronary calcification.
Treatment: It’s Not Just Medication
There’s no magic pill for CKD-MBD. Treatment is a three-legged stool:
- Diet: Cut phosphate. Avoid processed foods, colas, fast food, and packaged snacks. Read labels for "phos" in ingredients-those are added phosphate preservatives. Aim for 800-1000 mg per day.
- Binders: Take phosphate binders with every meal. They stick to phosphate in your gut and flush it out. Calcium-based binders work but carry heart risks. Non-calcium options like sevelamer are safer but cost more.
- Medications: Vitamin D supplements for deficiency. Calcimimetics like cinacalcet or etelcalcetide to trick the parathyroid gland into making less PTH. These are reserved for PTH over 500-800 pg/mL.
Dialysis helps remove phosphate-but only if it’s long enough. Four hours, three times a week is the minimum. Shorter sessions? Phosphate builds up between treatments.
What’s New in 2025?
Research is moving fast. A new injectable calcimimetic, etelcalcetide, reduces PTH by 45% weekly-better than daily cinacalcet. Anti-sclerostin drugs like romosozumab, which boost bone formation, are in phase 2 trials and show promise for reversing bone loss in CKD.
But the biggest shift? Starting earlier. New guidelines now recommend checking vitamin D and phosphate in Stage 3 CKD-not just Stage 5. Why? Because FGF23 starts rising 5-10 years before phosphate does. The damage begins long before you feel sick.
The Bottom Line
CKD-MBD isn’t a bone disease. It’s a whole-body disorder that links your kidneys, bones, and heart. Ignoring one part-like just lowering PTH without touching phosphate-makes things worse. The goal isn’t to fix numbers on a lab report. It’s to keep you alive longer, with fewer fractures, and a heart that still works.
If you have CKD, ask your doctor for these four tests every 6 months: phosphate, calcium, PTH, and vitamin D. Ask about your binder options. Ask if you’re on the right dose of vitamin D. Don’t wait until you break a hip or have a heart attack. The clock starts ticking the moment your kidney function drops below 60 mL/min.
Is CKD-MBD the same as renal osteodystrophy?
No. Renal osteodystrophy was the old term used only for bone changes in kidney disease. CKD-MBD is the modern term that includes bone problems, blood mineral imbalances, and vascular calcification. It’s a broader, more accurate description of what’s really happening in the body.
Can vitamin D supplements cure CKD-MBD?
No. Vitamin D helps, but it’s only one piece. Taking vitamin D won’t fix high phosphate or high PTH. It’s part of a team approach: diet, binders, meds, and dialysis. Studies show regular vitamin D reduces death risk by 15%, but only when combined with other treatments.
Why are calcium-based phosphate binders risky?
They lower phosphate, but they also add calcium to your blood. In CKD, excess calcium combines with phosphate to form crystals that stick to your arteries, heart valves, and lungs. This speeds up hardening of the arteries and raises heart attack risk. That’s why doctors limit calcium binders to 1500 mg of elemental calcium per day and often prefer non-calcium options.
Is low PTH dangerous?
Yes. Many think high PTH is the only problem. But when PTH drops too low (under 150 pg/mL), bone turnover slows to a crawl. This is called adynamic bone disease. Bones don’t renew themselves, so they become brittle and fracture easily-even if a bone scan looks normal. It’s silent, common in dialysis patients, and often missed.
How often should I get tested for CKD-MBD?
If you have Stage 3 or higher CKD, get your phosphate, calcium, PTH, and vitamin D checked every 6 months. If you’re on dialysis, every 3 months. Early detection is critical-changes in FGF23 and vitamin D can start years before phosphate rises. Waiting until you’re in Stage 5 means the damage is already advanced.
Can children with CKD develop CKD-MBD too?
Yes, and it’s especially serious. In children, CKD-MBD doesn’t just weaken bones-it stops growth. By Stage 5, many kids are 1.5 to 2 standard deviations below average height. That’s because bone formation is blocked. Aggressive treatment with vitamin D and phosphate control is needed early to prevent permanent stunting.
Lee M
January 2, 2026 AT 20:33Bryan Anderson
January 3, 2026 AT 09:31Austin Mac-Anabraba
January 3, 2026 AT 17:18LIZETH DE PACHECO
January 3, 2026 AT 23:04Kristen Russell
January 4, 2026 AT 02:29Bill Medley
January 6, 2026 AT 01:54Richard Thomas
January 6, 2026 AT 10:42Paul Ong
January 7, 2026 AT 10:39Andy Heinlein
January 9, 2026 AT 05:57Phoebe McKenzie
January 9, 2026 AT 07:31gerard najera
January 10, 2026 AT 23:04Stephen Gikuma
January 11, 2026 AT 11:01Bobby Collins
January 12, 2026 AT 20:59Layla Anna
January 13, 2026 AT 12:52Heather Josey
January 14, 2026 AT 14:41