 Nov, 20 2025
Nov, 20 2025
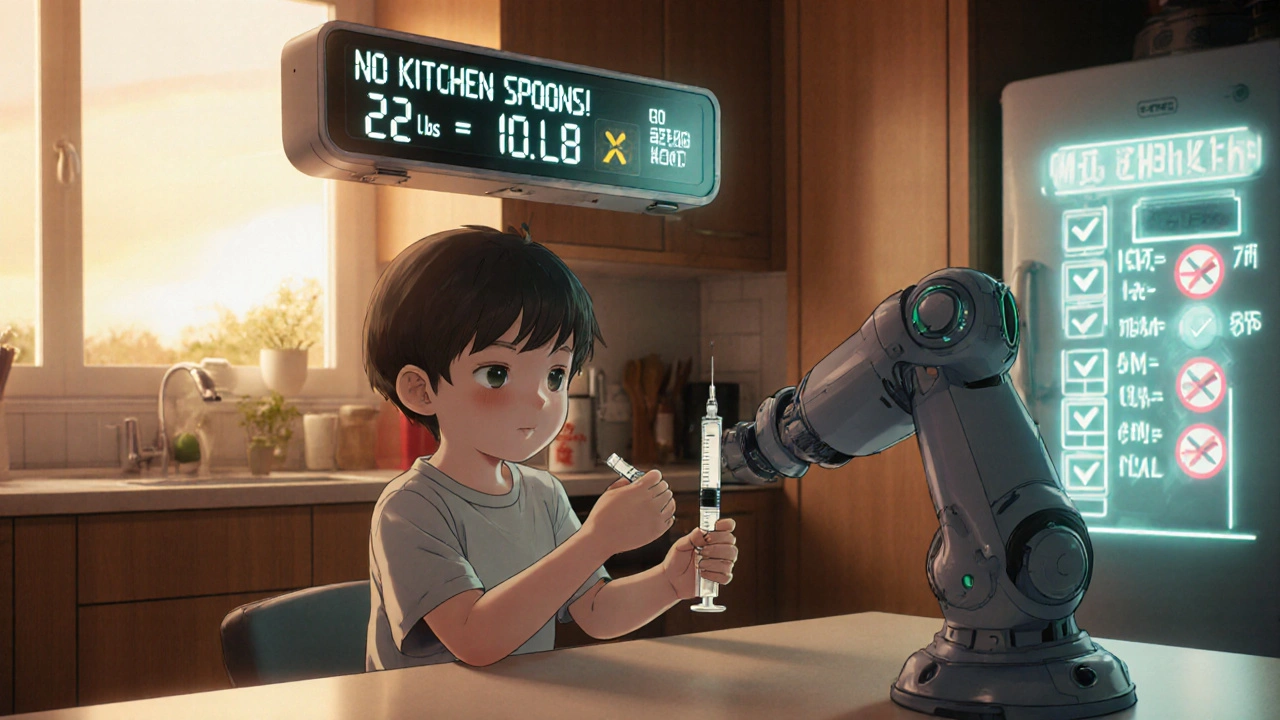
Getting the right dose of medicine for your child isn’t just important-it can be life-saving. Too little, and the infection won’t clear. Too much, and you could send your child to the emergency room. And here’s the scary part: 7 in 10 parents make a mistake when measuring liquid medicine at home. Most of these errors happen because people use kitchen spoons, misread labels, or don’t know the difference between mg and mL.
Why Milliliters (mL) Are the Only Measurement That Matters
Forget teaspoons and tablespoons. They’re not accurate. A kitchen teaspoon can hold anywhere from 3.9 to 7.3 milliliters-way off from the standard 5 mL. That’s why the CDC, the American Academy of Pediatrics, and the FDA all agree: all pediatric liquid medications must be measured in milliliters (mL).
Confusing 0.5 mL with 5 mL is a tenfold error. For a baby, that’s not a typo-it’s a medical emergency. Even a small mistake with antibiotics, fever reducers, or seizure meds can lead to hospitalization. That’s why you should never rely on the markings on a medicine bottle or the cap. Always use a proper measuring tool.
The Best Tools for Measuring Liquid Medicine
Not all measuring tools are created equal. Here’s what works-and what doesn’t:
- Oral syringes (1-10 mL): The gold standard. They’re accurate to within 1-2% and work best for doses under 5 mL. Parents using oral syringes get the dose right 94% of the time.
- Dosing cups (5-30 mL): Okay for older kids who can drink from a cup, but error rates jump to 68% for doses under 5 mL. Avoid them for babies and toddlers.
- Droppers (1-2 mL): Good for very small doses, like infant acetaminophen. Make sure the dropper came with the medicine-don’t swap it out.
- Medication spoons: Only use ones labeled with mL. Household spoons? Never.
Studies show that switching from dosing cups to oral syringes cuts errors by over 40%. Hospitals now give out free oral syringes at discharge. If your pharmacy didn’t give you one, ask for it. Most will provide one at no cost.
How to Use an Oral Syringe Correctly
It’s simple, but most people do it wrong. Here’s how to get it right every time:
- Shake the bottle well before measuring-especially antibiotics. If the medicine settles, your child gets less than the dose.
- Draw the medicine slowly into the syringe. Don’t rush.
- Hold the syringe vertically and check the level at eye level. Look at the bottom of the curve (the meniscus), not the top.
- Remove any air bubbles by tapping the syringe gently and pushing the plunger slightly to expel them.
- Give the medicine slowly into the side of the mouth, near the cheek. This reduces the chance your child will spit it out.
Pro tip: Use a permanent marker to mark common doses on the syringe. If your child takes 2.5 mL twice a day, draw a line at 2.5 mL. It’s a simple trick that cuts confusion and saves time.
Understanding Weight-Based Dosing
Most children’s medications are dosed by weight-not age. The label might say “5 mL per 10-15 kg,” but your child’s weight is listed in pounds. You need to convert.
Here’s the math: 1 kg = 2.2 lb. So if your child weighs 22 pounds, divide by 2.2. That’s 10 kg.
If the doctor prescribed 15 mg/kg of amoxicillin, and your child is 10 kg, that’s 150 mg total. If the medicine is 400 mg per 5 mL, then each mL has 80 mg. So 150 mg ÷ 80 mg/mL = 1.875 mL. Round to 1.9 mL and measure carefully.
Don’t guess. Use a calculator. Write it down. If you’re unsure, call your pharmacist. They’re trained to help with this.
Common Mistakes Parents Make (And How to Avoid Them)
- Mixing up mg and mL: One is a unit of weight (milligrams), the other is volume (milliliters). They’re not the same. Always double-check the label.
- Using the wrong syringe: Never use a syringe meant for injections. Only use oral syringes designed for medicine.
- Not shaking the bottle: Antibiotics and suspensions settle. If you don’t shake, your child gets a weaker dose.
- Using old medicine: Liquid antibiotics expire quickly-often within 14 days after opening. Check the label.
- Multiple caregivers using different tools: If grandma uses a spoon and mom uses a syringe, confusion happens. Keep one tool, and keep it in the same place.
One mom from Ohio told her story on a parenting forum: She gave her 18-month-old 5 mL of amoxicillin instead of 0.5 mL because she misread the decimal. The child got sick, rushed to the ER, and spent three days in the hospital. “I thought I was being careful,” she said. “I didn’t know how easy it was to mess up.”
What to Do If Your Child Refuses the Medicine
Over two-thirds of parents struggle with this. Kids spit out medicine. They gag. They cry.
Here’s what works:
- Use a flavored syrup version if available.
- Mix the dose with a small spoonful of applesauce, yogurt, or juice-only if the medicine allows it. Check the label or ask your pharmacist.
- Use a syringe to squirt the medicine slowly into the cheek pouch, not the front of the mouth.
- Let your child hold the syringe. Giving them control reduces resistance.
- Don’t force it. If your child throws up right after, don’t give another dose unless instructed by a doctor.
What’s Changing in Pediatric Dosing (2025 Update)
Things are getting better. In 2023, 78% of pediatric liquid medications came with mL-only labels-up from just 42% in 2015. The FDA is pushing for a new rule in 2025 that will require every pediatric liquid medicine to include a standard oral syringe in the box.
Smart tools are also coming. Philips Healthcare is testing dosing cups with built-in sensors that light up green when the right amount is poured. Apps like MedSafety use your phone’s camera to scan the bottle and show you exactly how much to give.
But the biggest change? Awareness. More pharmacies are printing dosing charts on the label. More pediatricians are handing out syringes. More hospitals are training parents before discharge.
What to Ask Your Pharmacist
Don’t leave the pharmacy without these questions:
- “Can you show me how to measure this dose with the syringe?”
- “Is this medicine supposed to be shaken before use?”
- “Can I get a free oral syringe if you didn’t give me one?”
- “What’s the concentration? Is it 100 mg/5 mL or 250 mg/5 mL?”
- “How long does this last once opened?”
Pharmacists are your best ally. They’ve seen every mistake. Ask them. Don’t be shy.
Final Checklist for Safe Dosing
Before you give any medicine to your child, run through this:
- ✅ Is the dose in mL, not tsp or tbsp?
- ✅ Are you using the syringe or cup that came with the medicine?
- ✅ Did you shake the bottle?
- ✅ Did you read the label at eye level?
- ✅ Did you confirm the weight-based dose with your doctor or pharmacist?
- ✅ Are you giving it to the cheek, not the front of the mouth?
- ✅ Did you write down the time and dose so you don’t double-medicate?
It takes less than a minute. But that minute could save your child’s life.
Can I use a kitchen teaspoon to measure my child’s medicine?
No. Kitchen teaspoons vary in size and can hold between 3.9 and 7.3 milliliters-far from the standard 5 mL. Using one can lead to under-dosing or dangerous overdosing. Always use a proper oral syringe or dosing cup marked in milliliters (mL).
What’s the difference between mg and mL?
Milligrams (mg) measure weight-how much active drug is in the medicine. Milliliters (mL) measure volume-how much liquid you give. A medicine might say 100 mg per 5 mL, meaning each 5 mL contains 100 mg of the drug. Confusing them is one of the most common causes of pediatric medication errors.
Why do I need to shake the medicine bottle before giving it?
Many liquid medicines are suspensions-solid particles mixed in liquid. If they settle, the top part has less medicine. Shaking ensures the drug is evenly distributed. Skipping this step can mean your child gets only half the dose, making treatment ineffective.
What should I do if my child spits out or throws up the medicine?
Don’t give another dose unless your doctor says to. If your child spits out most of it right away, you can try giving the full dose again. If they vomit within 15-20 minutes, check with your doctor. If it’s been longer than 20 minutes, the medicine was likely absorbed, and giving more could cause an overdose.
Are oral syringes better than dosing cups for babies?
Yes. For doses under 5 mL, oral syringes are far more accurate. Studies show dosing cups have error rates as high as 68% for small doses, while syringes are 94% accurate. Babies need precision-especially with antibiotics or fever reducers. Use a syringe until your child is old enough to drink from a cup reliably.
How do I convert my child’s weight from pounds to kilograms?
Divide the weight in pounds by 2.2. For example, a child weighing 22 pounds is 10 kg (22 ÷ 2.2 = 10). Most pediatric doses are calculated in mg per kg. If the dose is 15 mg/kg and your child is 10 kg, the total dose is 150 mg.
How long does liquid medicine last after opening?
Most liquid antibiotics last 7-14 days after opening. Check the label or ask your pharmacist. Some may say “discard after 14 days.” Even if it looks fine, it may lose potency. Never use expired medicine.
Can I use a syringe from a different medicine?
Only if it’s labeled for oral use and has the same scale (mL). Never use an insulin syringe or injection syringe-they’re designed for different purposes and can be dangerous. Always use the syringe provided with the medicine or buy a new one from the pharmacy.
Next Steps: What to Do Today
Don’t wait for an emergency. Take action now:
- Check all medicine bottles in your home. Are any still labeled with teaspoons?
- Call your pharmacy and ask for free oral syringes. Bring them home today.
- Write down your child’s weight in kilograms and keep it on your fridge.
- Make a quick dosing chart for your most-used medicines: name, dose in mL, frequency, and expiration date.
- Teach every caregiver-grandparents, babysitters, daycare staff-how to use the syringe. Show them, don’t just tell them.
Medication safety isn’t complicated. It’s about using the right tool, reading the label, and double-checking. Do those things, and you’re doing more than most parents. Your child’s health depends on it-and you’ve got this.
Darragh McNulty
November 20, 2025 AT 19:38Willie Doherty
November 21, 2025 AT 05:56David Cusack
November 22, 2025 AT 14:12Elaina Cronin
November 23, 2025 AT 19:56Eliza Oakes
November 25, 2025 AT 01:28Sammy Williams
November 26, 2025 AT 08:35Cooper Long
November 27, 2025 AT 03:46Sheldon Bazinga
November 28, 2025 AT 21:34Sandi Moon
November 30, 2025 AT 10:12Kartik Singhal
December 2, 2025 AT 03:47Chris Vere
December 2, 2025 AT 06:41Pravin Manani
December 3, 2025 AT 02:26