 Feb, 3 2026
Feb, 3 2026
When someone leaves the hospital, their medication list often changes. Drugs may be added, stopped, or dosed differently. But here’s the problem: medication reconciliation doesn’t always happen after discharge. In fact, studies show that 30% to 70% of patients leave the hospital with a medication list that doesn’t match what they were actually taking before admission. This mismatch is one of the leading causes of preventable readmissions and dangerous side effects.
Why Medication Reconciliation Matters
Medication reconciliation isn’t just paperwork. It’s a safety checkpoint. Think of it like double-checking your GPS route before you start driving. If the app says to turn left but your map shows a right turn, you could end up lost - or worse. The same thing happens with medications. A patient might have been on blood pressure medicine before the hospital, but during their stay, doctors stopped it. If no one checks whether they should restart it when they go home, their blood pressure could spike. Or worse, they might be sent home with a new drug that interacts dangerously with something they’re still taking.
The National Quality Forum calls this process NQF 0097. It’s not optional. Medicare and Medicaid require it. If your provider doesn’t document that they reviewed your medications within 30 days of discharge, it can hurt their reimbursement - and more importantly, it puts you at risk. According to the Agency for Healthcare Research and Quality, medication errors after discharge cause up to 50% of avoidable adverse drug events. That’s why the American Board of Internal Medicine says medication reconciliation is one of the top three things that can prevent hospital readmissions.
What Happens During Medication Reconciliation
The process is simple in theory but tricky in practice. It involves comparing three things:
- What you were taking before you went to the hospital
- What you were given while you were hospitalized
- What you’re supposed to take when you go home
This isn’t just about pills. It includes vitamins, supplements, creams, eye drops, and herbal products. Many patients don’t think of these as “medications,” but they can cause serious interactions. For example, St. John’s Wort can interfere with blood thinners. A daily fish oil supplement can increase bleeding risk when combined with aspirin.
The goal is to find discrepancies - drugs that were stopped but shouldn’t have been, new drugs that weren’t explained, or doses that were changed without clear instructions. The best providers don’t just guess. They pull your full medication history from pharmacy records, electronic health systems, and direct conversations with you or your caregiver.
Who Should Do It - And How
Traditionally, doctors or nurses handled this. But research shows that’s not enough. A 2023 study in the Journal of the American College of Clinical Pharmacy found that when pharmacists led the reconciliation process, medication discrepancies dropped by 32.7%. Readmissions fell by 28.3%. Why? Pharmacists are trained to spot interactions, understand dosing nuances, and ask the right questions.
There are two main ways this is done:
- Standalone reconciliation (CPT II 1111F): No office visit needed. Your primary care provider or pharmacist can call you, video chat, or even send a secure message through your patient portal. They review your current meds against your discharge list and document the match. This is flexible but doesn’t come with a payment incentive.
- Transitions of Care (TRC) visit (CPT 99495/99496): You have an in-person appointment within 30 days of discharge. This is billable, so providers are more likely to schedule it. But here’s the catch: only one provider can bill for this per hospital stay. If your PCP and your cardiologist both try to bill, only one gets paid. This creates tension - and sometimes, no one does the job.
The most effective systems embed pharmacists into discharge teams. A 2022 JAMA Internal Medicine study showed that hospitals with pharmacists on discharge rounds reduced medication errors by 37%. These pharmacists don’t just hand out lists. They ask: “Did you fill your new prescription?” “Are you taking your old meds too?” “Do you know why you’re on this new pill?”
The Biggest Barriers
Even though the process is proven, it still fails often. Why?
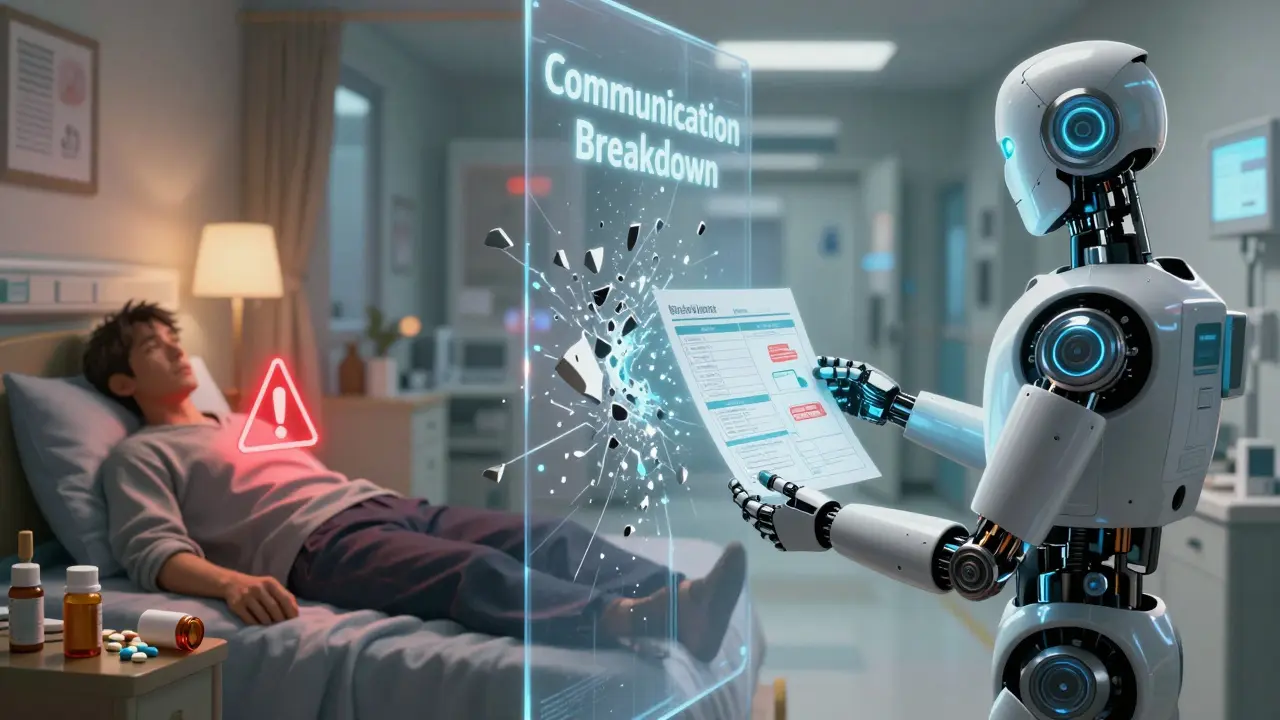
- Fragmented records: Your hospital’s electronic system might not talk to your pharmacy’s system or your doctor’s office. One study found 68% of hospitals struggle with this.
- Time pressure: Primary care doctors say they don’t have enough time in a 15-minute visit to properly review meds. One 2021 study found 82% of PCPs cited time as a major barrier.
- Poor communication: Discharge summaries often don’t clearly list changes. A patient might get a 10-page discharge packet with no summary of what was changed - and why.
- Patients don’t speak up: Many don’t realize they should question their meds. They assume the hospital knows best.
One common scenario: A patient with atrial fibrillation gets stopped on warfarin during hospitalization because they had surgery. At discharge, the cardiology team forgets to restart it. The PCP, focused on diabetes, doesn’t know it was ever stopped. The patient goes home and has a stroke. This isn’t rare. It’s exactly the kind of failure medication reconciliation is designed to prevent.
How to Make Sure It’s Done Right
If you or a loved one is being discharged, here’s what you can do:
- Bring a list: Before you leave the hospital, write down every medication you take - including doses, times, and reasons. Include supplements and OTC drugs.
- Ask for a written summary: Request a one-page summary of changes made during your hospital stay. It should say: “Stopped,” “Started,” “Changed,” with clear reasons.
- Confirm the pharmacy: Call your pharmacy 24 hours after discharge. Ask if they received your new prescriptions. If they haven’t, the discharge order might not have been sent.
- Set a follow-up: Schedule a medication review with your primary care provider or pharmacist within 7 days. Don’t wait 30 days. The first week is when most errors happen.
- Use tech: Many apps now let you scan pill bottles and sync your list to your health record. Try one. They’re free and accurate.
Providers, too, need to change. The most successful clinics now use automated EHR alerts that flag high-risk changes - like stopping an anticoagulant or starting a new kidney-toxic drug. One 2023 study showed these alerts cut reconciliation errors by 29%.
The Bottom Line
Medication reconciliation isn’t a bureaucratic box to check. It’s a lifeline. Every year, medication errors after discharge cost the U.S. healthcare system over $21 billion. And for families, the cost is far greater - in fear, in recovery time, in lost independence.
The fix isn’t complicated. It’s about communication, clarity, and accountability. Pharmacists who lead this process save lives. Systems that automate alerts prevent mistakes. Patients who ask questions protect themselves.
If you’ve just left the hospital, don’t assume everything’s been taken care of. Ask for your medication summary. Double-check your prescriptions. Make sure someone - a doctor, a pharmacist, a nurse - has looked at your list side by side with what you were taking before. Because when it comes to your meds, confusion kills. Clarity saves.
What exactly is medication reconciliation after hospital discharge?
Medication reconciliation is the process of comparing a patient’s current home medications with the medications prescribed at discharge from the hospital. The goal is to identify and fix any differences - such as medications that were stopped, changed, or added - to prevent harmful errors. This includes prescription drugs, over-the-counter medications, vitamins, supplements, and topical treatments.
Who is responsible for performing medication reconciliation?
While doctors or nurses may start the process, research shows pharmacists are the most effective at completing it. Pharmacists have specialized training in drug interactions, dosing, and adherence. Hospitals and clinics with pharmacist-led reconciliation programs see 30% fewer medication errors and lower readmission rates. Primary care providers must also confirm and document the reconciliation within 30 days.
Is medication reconciliation required by law?
Yes. The Centers for Medicare & Medicaid Services (CMS) requires it as part of quality reporting standards (NQF 0097). Providers must document that medication reconciliation occurred within 30 days of discharge. Failure to do so can reduce Medicare reimbursements under the Merit-based Incentive Payment System (MIPS). It’s not optional - it’s a key measure of care quality.
Can I do anything to help ensure my medications are reconciled?
Absolutely. Before discharge, bring a complete list of all your medications - including doses and why you take them. Ask for a written summary of changes. Call your pharmacy within 24 hours to confirm prescriptions were filled. Schedule a follow-up appointment with your primary care provider or pharmacist within a week. Don’t wait - most errors happen in the first few days after leaving the hospital.
Why do so many patients still have medication errors after discharge?
The biggest reasons are poor communication between providers, fragmented electronic health records, and lack of time during follow-up visits. Many discharge summaries don’t clearly explain what changed or why. Patients often don’t understand their new regimen. And without a pharmacist involved, subtle but dangerous interactions go unnoticed. Studies show 73% of hospitals have weak communication protocols, and 82% of primary care doctors say they don’t have enough time to do it right.
Caleb Sutton
February 3, 2026 AT 17:41The system is rigged. They don't want you to know what you're really on. That 'reconciliation'? It's a smokescreen. They change your meds, bury the paper trail, and when you crash, it's 'patient noncompliance.' I've seen it. My uncle died because his blood thinner got dropped and no one told him. The hospital's EHR didn't even log the change. Someone's covering up. This isn't incompetence. It's profit-driven negligence.