 Dec, 16 2025
Dec, 16 2025
Running out of your blood pressure pill on a Saturday? Or paying $50 for a 30-day supply of a generic medication when you could get 90 days for under $20? Most people don’t realize they’re overpaying for prescriptions because they’re using only one pharmacy - and missing out on smart ways to cut costs. The truth is, you don’t have to choose between mail-order and your local pharmacy. You can use both - and save hundreds a year.
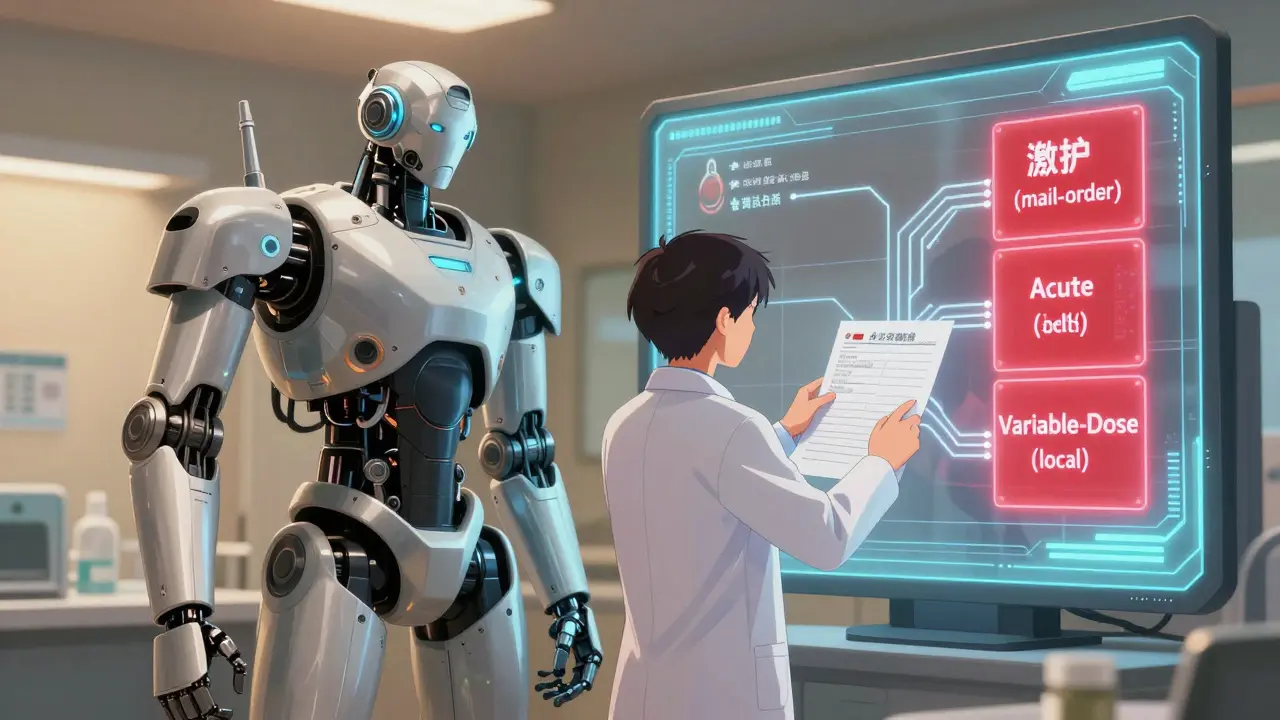
Know Which Medications Belong Where
Not all medications are created equal when it comes to cost and timing. Start by sorting your prescriptions into three groups: maintenance, acute, and variable-dose.- Maintenance meds are the ones you take every day, long-term - like metformin for diabetes, lisinopril for high blood pressure, or levothyroxine for thyroid issues. These are perfect for mail-order.
- Acute meds are short-term: antibiotics, painkillers after surgery, or steroid packs. These need to be picked up fast - local pharmacy only.
- Variable-dose meds are the tricky ones: antidepressants, anticonvulsants, or insulin if your dose changes often. Stick with your local pharmacy until things stabilize.
Mail-order is designed for steady, predictable use. It’s not built for changes. If your doctor adjusts your dose, you could end up with a box of pills you can’t use - and waste money. One user on Reddit lost $65 because their mail-order pharmacy kept sending the old dose after a change. Local pharmacists can catch that right away.
Check Your Insurance’s Real Costs
Your insurance plan might make it look like mail-order is cheaper - but that’s not always true. Many people assume they have to use the mail-order service tied to their plan. They don’t.Call your insurer and ask: "What’s my copay for a 90-day supply of [medication name] at a local pharmacy?" You’d be surprised. CVS, Walmart, and Kroger all offer 90-day generic prescriptions at prices matching mail-order - sometimes even lower. Walmart’s $10 generic program (for 90 days) beats most mail-order copays. CVS’s $4/$10/$25 program works the same way.
Here’s a real example: A Medicare Part D plan charges $45 for a 30-day supply of a Tier 3 brand-name drug at a local pharmacy. The same drug, 90-day supply, through mail-order? $115. That’s $115 for 90 days - or $1.28 per day. But if you get the 90-day supply at your local CVS? Still $115. Same price. No shipping wait. Same savings. You just have to ask.
Mail-Order Isn’t Always Faster - Or Cheaper
Most mail-order pharmacies take 7 to 14 days to deliver. That’s fine if you’re planning ahead. But if you run out on a Friday and your doctor’s office is closed? You’re stuck.Also, not all medications save you money through mail-order. A 2007 study in the Journal of Managed Care Pharmacy found that cardiovascular drugs saved users 35% with mail-order. But dermatological drugs? Only 8.7%. Some specialty drugs - like injectables or biologics - actually cost more through mail-order because of handling fees.
And temperature-sensitive meds? Insulin, certain antibiotics, and biologics can lose potency if shipped in extreme heat or cold. The FDA warns that improper shipping can reduce effectiveness. Local pharmacies store and transport these safely. Mail-order? You’re rolling the dice.
Use Your Local Pharmacist as a Free Consultant
Your local pharmacist isn’t just there to hand out pills. They’re trained to spot interactions, suggest cheaper alternatives, and tell you when a generic version is available.One study found 78% of patients preferred face-to-face advice from a pharmacist over phone support from a mail-order center. That’s huge. If you’re on five or more meds, a pharmacist can review them once a year and often find savings you didn’t know existed. The American Pharmacists Association says 40% of patients could save $200 or more annually just by talking to their local pharmacist.
Build a relationship. Go in during slow hours. Ask: "Is there a cheaper way to get this?" or "Can I get a 90-day supply here instead of waiting for mail?" Most pharmacists will help - they want you to stick with them.
Set Up a Refill System That Works
The biggest mistake people make? Waiting until they’re out of pills to refill. That’s how you end up in an emergency room because your blood pressure spiked.Here’s what works: Set calendar reminders 10 to 14 days before your mail-order meds run out. That gives you time to order, ship, and receive - no rush. Use your phone’s calendar app. Label the reminder: "Amlodipine 5mg - order 90-day refill".
For local pharmacy meds, keep a small stash - maybe 5 to 7 extra pills - as a buffer. Don’t wait until the last tablet to refill. If you’re on a tight budget, ask your pharmacist about free or low-cost delivery options. Many local pharmacies now offer same-day delivery through apps like DoorDash or Instacart.

Watch for Plan Changes - They Happen Often
Insurance plans change every year. What saved you $300 last year might cost $50 more this year. Don’t assume your system still works.Every October, during open enrollment, check your plan’s formulary update. Look for changes in:
- Which drugs are in which tier
- Mail-order vs. retail copays
- Whether 90-day fills are even allowed at local pharmacies
GoodRx’s 2023 survey found 41% of users had unexpected cost increases because their plan changed without notice. Don’t be one of them. Print your plan’s formulary or save the PDF. Compare it every year.
What’s Next? Integrated Systems Are Coming
The pharmacy world is changing. UnitedHealthcare’s Optum Perks and Express Scripts’ Pharmacy Choice program now let you switch between mail-order and local pharmacies without losing your refill history. Medicare’s 2024 Part D redesign is standardizing 90-day pricing across channels.By 2025, most commercial plans will have unified refill systems. That means your doctor’s EHR might soon suggest: "This medication is cheaper via mail-order. Would you like to switch?" But until then, you’re the one in control.
Don’t wait for automation. Start now. Sort your meds. Call your insurer. Talk to your pharmacist. Set reminders. You don’t need to be a health expert to save money - you just need to be organized.
One user in Manchester saved $427 last year by switching their blood pressure pill to mail-order and keeping their inhaler local. They didn’t change doctors. Didn’t switch plans. Just used both systems the way they were meant to be used.
You can too.
Brooks Beveridge
December 18, 2025 AT 07:03Love this breakdown. I’ve been using mail-order for my metformin and local for my insulin-no more panic runs at 11 PM on a Sunday. Also, my pharmacist noticed my generic lisinopril was suddenly $35, but the 90-day at Walmart was $10. She called my insurer and got it switched. Free advice is the best kind. 🙌
Sachin Bhorde
December 19, 2025 AT 07:19Bro, this is gold. I was paying $80 for my atorvastatin till I found out CVS has a $10 90-day for generics. My local pharma guy even gave me a free pill splitter for my 20mg tabs. Pro tip: ask for samples when you’re switching. They always have ‘em. Also, use GoodRx + pharmacy coupons-it’s like cheat codes for your meds. 💪
Josh Potter
December 19, 2025 AT 13:10STOP WASTING MONEY. Mail-order is a trap if you’re not planning ahead. I ran out of my anxiety med because the damn package got stuck in transit during a snowstorm. Got it at Walgreens same day for $12. Your insurance doesn’t care if you’re in crisis-they care about their margins. Be the boss of your own health. 🤬
Evelyn Vélez Mejía
December 19, 2025 AT 23:36One cannot overstate the epistemological significance of decentralized pharmaceutical access. The bifurcation of maintenance versus acute pharmacotherapy represents not merely an economic strategy, but a hermeneutic reclamation of bodily autonomy from corporate pharmacy-industrial complexes. One must interrogate the ontological assumptions embedded in ‘convenience’-is it truly convenience, or merely the commodification of vulnerability? I, for one, refuse to be a passive node in the supply chain. 🌿
Victoria Rogers
December 20, 2025 AT 04:15Yeah right. Like anyone cares about this. You think your little ‘system’ matters? The system is rigged. My insurance raised my mail-order copay by $60 last year and I had to beg my pharmacist to even give me the 90-day option. Walmart’s $10 program? Only if you’re on Medicaid. Everyone else gets screwed. This post is just feel-good fluff for people who still have health insurance. 🙄
Anna Giakoumakatou
December 21, 2025 AT 09:03How quaint. You’re treating pharmacy logistics like a lifestyle blog. Did you also learn to ‘optimize your vitamin D intake’ from a TikTok? The fact that you need a flowchart to manage your meds speaks volumes. I just take what my doctor prescribes and pay what I’m told. Simplicity is elegance. You’re overcomplicating the inevitable.
Erik J
December 21, 2025 AT 14:42Interesting. I’ve been using mail-order for everything since 2021. Never had an issue. But I’m curious-how often do people actually get their mail-order meds delayed? I’ve only had one late shipment in 3 years. Maybe it’s regional? I’m in the Midwest.
BETH VON KAUFFMANN
December 22, 2025 AT 15:30Ugh. This is the same recycled content every year. You’re missing the real issue: PBMs. The middlemen. They’re the ones jacking up prices, not the pharmacies. Mail-order? It’s just a PBM shell game. Your ‘savings’ are illusions created by formulary tier manipulation. If you want real savings, lobby for PBM transparency laws. Stop optimizing your pill schedule like it’s a spreadsheet.
Raven C
December 23, 2025 AT 15:55How… pedestrian. You speak of ‘$10 generics’ as if they are a moral triumph. But what of the dignity of care? The human connection? The quiet, dignified exchange between patient and pharmacist-reduced to a transactional checklist? I weep for the erosion of the sacred pharmaceutical relationship. And you call this ‘saving money’? No. You’ve sold your soul to the algorithm.
Donna Packard
December 24, 2025 AT 08:49This helped me so much. I used to panic every time I ran out of my thyroid med. Now I set a reminder 2 weeks before. And I started asking my pharmacist about alternatives-I saved $150 last year. It’s not hard, just a little effort. 💛
Patrick A. Ck. Trip
December 25, 2025 AT 14:05Thank you for this thoughtful and meticulously structured exposition. While I concur with the majority of the operational recommendations, I would respectfully posit that the temporal coordination of refill cycles may benefit from integration with calendar-based health analytics platforms-such as Apple Health or Google Fit-to ensure predictive adherence modeling. A minor oversight in the original text, but one that could enhance scalability for digitally engaged users.
Virginia Seitz
December 27, 2025 AT 14:02My pharmacist gave me free delivery for my blood pressure pills. I just asked. 😊
Peter Ronai
December 27, 2025 AT 22:58Oh wow. You actually think this is groundbreaking? I’ve been doing this since 2017. And you know what? The people who need this info the most-seniors on fixed incomes-are the ones who don’t read Reddit. This post is just preaching to the choir. Meanwhile, Big Pharma laughs all the way to the bank. 🤡