 Dec, 7 2025
Dec, 7 2025
Restarting a medication after taking a break can be deadly-even if you’ve done it safely before. This isn’t about being careless. It’s about biology. Your body forgets how to handle the drug. The tolerance you built up? Gone. But your brain still remembers the dose that used to work. That mismatch is what kills people.
Why Your Body Can’t Handle the Same Dose Anymore
When you stop taking a medication like an opioid, benzodiazepine, or even certain antidepressants, your body begins to reset. Within days, your brain reduces the number of receptors that respond to the drug. Your liver slows down how fast it processes it. Your lungs become more sensitive to its depressant effects. All of this happens quietly, without warning.Take methadone, for example. If you stop for just 3 to 5 days, your tolerance drops dramatically. That’s not a guess-it’s what the Washington State Department of Health confirmed in their official overdose prevention guide. The same thing happens with oxycodone, heroin, and even prescription sleep aids. You might think, ‘I took 40mg before and I was fine.’ But now, 40mg could stop your breathing. You’re not stronger. You’re weaker to the drug.
This isn’t rare. The Jackson Laboratory documented the case of actor Philip Seymour Hoffman, who died of an overdose after 23 years without using heroin. He wasn’t a new user. He was someone who’d been clean for decades. But his body had forgotten how to cope. He took the same dose he used to, and it killed him.
Which Medications Carry the Highest Risk?
Not all medications are equal when it comes to restarting after a break. Some are far more dangerous than others.- Opioids (oxycodone, fentanyl, methadone, heroin): Highest risk. Even a single dose after a few days off can cause fatal respiratory depression. Fentanyl is especially deadly because it’s 50 to 100 times stronger than morphine. A tiny amount can be lethal if your body isn’t prepared.
- Benzodiazepines (alprazolam, diazepam, clonazepam): These slow down your central nervous system. After a break, your brain becomes hypersensitive. Restarting at your old dose can cause extreme drowsiness, confusion, or breathing failure.
- Antidepressants (MAOIs and SSRIs): Restarting MAOIs like phenelzine too soon after stopping an SSRI like sertraline can trigger serotonin syndrome-a life-threatening spike in body temperature, heart rate, and blood pressure. The washout period between these drugs can be weeks, not days.
- Quetiapine and other antipsychotics: These can cause dangerous drops in blood pressure when restarted at old doses. The Medicines Learning Portal warns that restarting at full dose after just one week off can lead to fainting, falls, or heart rhythm problems.
And here’s the worst part: many people don’t even realize they’re at risk. They think, ‘I just took a break for a few days because I was sick,’ or ‘I stopped because I ran out of pills.’ They don’t connect the dots between their break and the danger ahead.
How to Restart Safely: The ‘Start Low, Go Slow’ Rule
There’s one rule that saves lives: start low, go slow. It’s not a suggestion. It’s a medical standard.The Calgary Clinical Pharmacology service and the Washington State Department of Health both say the same thing: if you’re restarting an opioid after a break, begin at 25% to 50% of your previous daily dose. For someone who used to take 60mg of oxycodone a day, that means starting at 15mg or less. Then wait at least 24 hours before taking another dose.
For benzodiazepines, the same principle applies. If you were on 10mg of diazepam daily, start with 2.5mg. For quetiapine, start with 25mg-even if you used to take 200mg. Let your body adjust. Don’t rush.
And don’t assume your old dose is safe just because you feel fine after a few days. Tolerance doesn’t come back overnight. It takes weeks for your body to rebuild its sensitivity to these drugs. Pushing the dose too fast can lead to hospitalization-or worse.
Medical Supervision Isn’t Optional-It’s Essential
Restarting medication alone is like driving blindfolded. You might get lucky. But you’re gambling with your life.Studies show that patients who restart opioids under medical supervision have an 87% success rate in avoiding overdose. Those who do it on their own? Only 42%. That’s not a small difference. That’s life or death.
Doctors don’t just adjust doses. They monitor you. They check your breathing rate. They look for pinpoint pupils (a sign of opioid overdose). They watch for extreme drowsiness or confusion. They have naloxone ready-because if your breathing slows, they can reverse it immediately.
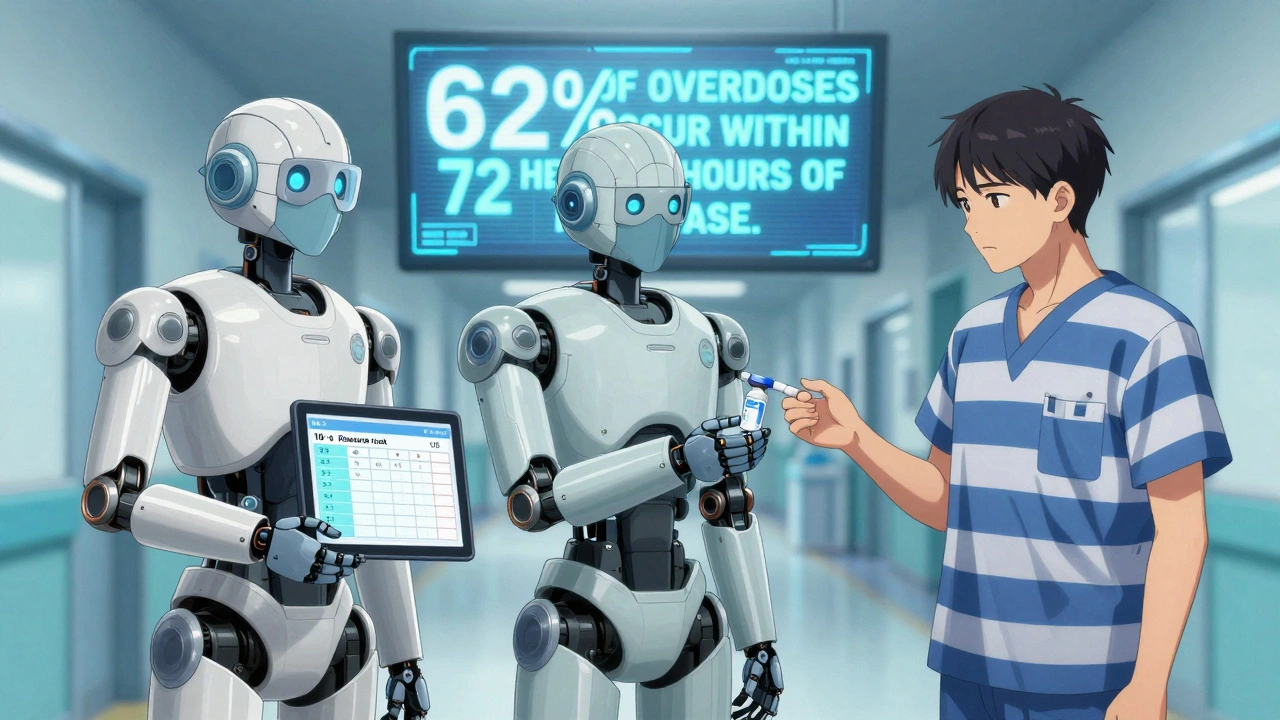
And if you’re coming out of jail, a rehab center, or a hospital stay? Your risk is highest. Washington State data shows 62% of fatal opioid overdoses happen within 72 hours after release. That’s when tolerance is lowest and access to help is often gone.
Ask your doctor for a restart plan. If they don’t have one, ask for a referral to a pain management clinic or addiction specialist. This isn’t weakness. It’s wisdom.
What You Must Have Before Restarting
There are three non-negotiable items you need before restarting any high-risk medication:- Naloxone: This is the opioid overdose reversal drug. It’s not just for addicts. It’s for anyone restarting opioids-even if they’re prescribed. Keep it in your home. Give one to a friend or family member. Know how to use it. The Washington State guidelines say: ‘This resource should be shared with a friend or family member.’
- A buddy system: Don’t restart alone. Have someone with you for the first 24 to 48 hours. Someone who can call 999 if you stop breathing, can’t wake up, or turn blue.
- A clear timeline: Know how long you’ve been off the drug. If it’s been less than 7 days, assume your tolerance is nearly zero. If it’s been 30 days or more, you’re starting almost from scratch.
And never mix your medication with alcohol, sleep aids, or other sedatives. That’s a recipe for respiratory arrest. Even a glass of wine can turn a safe dose into a fatal one.
What to Watch For: Signs of Overdose
You need to recognize the warning signs before it’s too late:- Slow or shallow breathing (less than 12 breaths per minute)
- Pinpoint pupils (tiny dots in the center of your eyes)
- Unresponsiveness-you can’t wake the person up, even with loud shouting or shaking
- Blue or gray lips and fingernails (sign of low oxygen)
- Extreme drowsiness or confusion that gets worse
If you see any of these, act immediately. Give naloxone if you have it. Call 999. Don’t wait. Don’t hope it passes. Overdose doesn’t care if you’re ‘just trying to get back on track.’
What’s New in 2025: Better Tools, Better Protection
The field is changing. In February 2024, the American Society of Addiction Medicine released new guidelines that use a 10-point scoring system to calculate safe restart doses based on how long you’ve been off the drug, your previous dose, and your health history. It’s not perfect-but it’s better than guessing.Also in 2023, Johns Hopkins found that giving extended-release naltrexone (a medication that blocks opioids) before restarting opioids reduced overdose risk by 73% in the first 30 days. It’s not widely available yet, but it’s coming.
And now, wearable devices are being tested that monitor your breathing and automatically inject naloxone if your rate drops dangerously low. These are in Phase 3 trials and could be available within the next year.
The CDC’s 2024 Overdose Prevention Plan now lists standardized restart protocols as one of its top three priorities. That means hospitals, prisons, and clinics are being forced to do this right. But until then, you can’t wait for the system to catch up. You have to protect yourself.
Final Reality Check
This isn’t about being scared. It’s about being smart. People who restart medication after a break aren’t weak. They’re trying to get better. But biology doesn’t care about your intentions. It only cares about what’s in your bloodstream and how your body reacts to it.If you’re thinking about restarting a medication after a break, don’t do it alone. Don’t rely on memory. Don’t trust how you ‘felt’ before. Your body has changed. Your tolerance is gone. And the dose that once worked could kill you now.
Start low. Go slow. Get help. Have naloxone. Tell someone. These aren’t steps. They’re your lifeline.
How long does it take to lose tolerance to opioids after stopping?
Tolerance to opioids drops quickly-within 3 to 5 days for short-acting ones like heroin or oxycodone. For longer-acting drugs like methadone, it can take 7 to 10 days. After 30 days off, your tolerance is nearly gone. That’s why restarting at your old dose is so dangerous.
Can I restart my medication on my own if I feel fine?
No. Feeling fine doesn’t mean your body is ready. Tolerance is invisible. You can feel completely normal and still be at high risk for overdose. Medical supervision reduces overdose risk by more than 40%. Don’t risk your life on how you feel.
Is naloxone only for people who use street drugs?
No. Naloxone is for anyone restarting opioids-even if they’re prescribed. In fact, 62% of fatal opioid overdoses happen to people who were in treatment or recently released from jail. They weren’t using street drugs. They were restarting their own medication. Naloxone saves lives regardless of how the drug was obtained.
What if I’m restarting an antidepressant like sertraline or venlafaxine?
If you were on an MAOI (like phenelzine) before, you must wait at least 14 days before restarting sertraline or venlafaxine-otherwise you risk serotonin syndrome. For other antidepressants, restart at a low dose and increase slowly over weeks. Always check with your doctor. Some medications have very specific washout periods.
Why is restarting after jail or hospital so dangerous?
Because your tolerance drops fast in those settings, and you’re often discharged without a plan. You may have been on a high dose before, but during your stay, you were given nothing-or a much lower dose. When you leave and take your old dose again, your body can’t handle it. That’s why 62% of fatal overdoses happen within 72 hours of release.
Can I use my old prescription to restart?
Never. Your old prescription was written for a different version of you. Your tolerance is gone. Your body is different. Taking the same dose can be fatal. Always see your doctor before restarting. They may need to write a new prescription with a lower starting dose.
Are there any medications that are safe to restart without help?
Generally, no. Even medications like ibuprofen or thyroid pills should be restarted under medical guidance after a long break. But the highest risk is with opioids, benzodiazepines, MAOIs, and certain antipsychotics. If your medication is any of those, medical supervision is not optional-it’s life-saving.
Stacy Tolbert
December 7, 2025 AT 16:53I restarted my oxycodone after a week off because I thought I'd be fine. I wasn't. Ended up in the ER with breathing so shallow my roommate thought I was asleep. Naloxone saved me. Don't be me.
Just... start low. Please.
Raja Herbal
December 9, 2025 AT 09:13Oh wow, so now we're treating adults like toddlers who can't remember their own dosages? 'Start low, go slow' - yeah, because obviously your body is a magic box that forgets everything after a weekend vacation.
Meanwhile, my cousin’s been on methadone for 12 years and took a 10-day break for a surgery. Took his normal dose. Fine. No drama. Maybe biology isn’t the only thing at play here.
Iris Carmen
December 10, 2025 AT 15:12so like... if i took a 3 day break cause i was sick, and i feel totally normal now, can i just take my usual 20mg? i mean, i dont wanna die but also i dont wanna be that guy who takes 5mg and feels nothing for a week lmao
also pls tell me where to get naloxone without looking like a junkie at the pharmacy
Rich Paul
December 11, 2025 AT 00:45Y’all are missing the pharmacokinetics here. Tolerance isn’t just receptor downregulation - it’s CYP450 enzyme induction, P-glycoprotein efflux changes, and GABA-A subunit plasticity. When you stop, hepatic clearance drops by 40-60% within 72 hours, and mu-opioid receptor density plummets faster than your ex’s text replies.
And don’t even get me started on the allosteric modulation of benzodiazepine binding sites. You think your brain ‘forgets’? Nah. It’s rewiring. Like a neural OS rebooting without the patch notes.
Start at 25%? That’s not ‘cautious,’ that’s just math. The CDC’s 2024 protocol uses a weighted risk score based on half-life, BMI, and prior episodes of respiratory depression. You’re not ‘guessing’ - you’re doing a Bayesian dose calibration. Do the work.
Katherine Rodgers
December 12, 2025 AT 14:07Wow. A whole 1,200-word essay on how not to kill yourself with your own prescription. Did we forget to mention ‘don’t breathe’ in the title?
Also, ‘naloxone for everyone’? Next you’ll tell me we need fire extinguishers in every bathroom because someone might light a candle and forget. I mean, sure, it’s nice you’re worried - but is this really the best use of public health resources? Maybe stop writing prescriptions for people who forget how to take pills?
Lauren Dare
December 13, 2025 AT 17:57Let me get this straight - you’re telling people to restart opioids with medical supervision, have a buddy, carry naloxone, and avoid alcohol... but you’re not telling them to stop taking opioids?
Because let’s be real - this whole post reads like harm reduction porn. ‘Here’s how to not die while doing the thing that’s slowly killing you.’
Why not just say: ‘If you’re restarting this, you haven’t quit. And you’re not ready.’
Mona Schmidt
December 14, 2025 AT 12:06Thank you for writing this with such clarity and compassion. I work in community mental health, and I see too many people discharged from hospitals or jails with no plan - just a script and a prayer. The ‘start low, go slow’ rule isn’t just medical advice - it’s dignity. It’s saying: ‘Your life matters enough to be handled carefully.’
To those reading this who feel ashamed for needing help: you’re not weak. You’re human. And your body isn’t broken - it’s adapting. Give it the space to heal. Reach out. Ask for the plan. You deserve that safety net.
Guylaine Lapointe
December 15, 2025 AT 03:30Wow. So now we’re treating people like fragile glass figurines that shatter if they take their own medicine? This is the kind of paternalistic nonsense that makes people avoid doctors entirely.
If you’re too scared to restart your own prescription, maybe you shouldn’t have been on it in the first place. This isn’t a public service announcement - it’s fearmongering dressed as science. Next they’ll tell us not to drive because we might get in an accident after a nap.
Sarah Gray
December 15, 2025 AT 03:51Let’s be honest - this post is a glorified liability waiver for pharmaceutical companies. You’re not protecting people. You’re protecting the system that keeps them dependent.
And don’t get me started on ‘naloxone for everyone.’ That’s not prevention - that’s enabling. If you’re restarting opioids because you ‘felt better’ after a break, you’re not healing. You’re chasing a ghost.
Real recovery doesn’t need a dosing schedule. It needs a reason to quit.
Suzanne Johnston
December 16, 2025 AT 03:56There’s a quiet tragedy here - not in the pharmacology, but in the silence. We don’t talk about how hard it is to admit you need your medication again. We don’t talk about how shame makes people restart alone. We don’t talk about how the system abandons people the moment they leave the hospital or prison.
This post isn’t about dosing. It’s about belonging. It’s saying: ‘You’re not alone. You’re not a failure. You’re still worth saving.’
And if that makes some people uncomfortable? Good. Maybe it’s time we stopped pretending recovery is just about willpower.