 Jan, 14 2026
Jan, 14 2026
When your kidneys start to fail, your body doesn’t just slow down-it starts to swell. Edema in chronic kidney disease (CKD) isn’t just a nuisance. It’s a sign your body is drowning in fluid it can’t get rid of. You might notice your ankles puffing up, your shoes feeling tighter, or your face looking puffy in the morning. For many people with stage 3 or worse CKD, this swelling doesn’t go away with a good night’s sleep. It gets worse. And if left unchecked, it can lead to hospital visits, heart strain, and even faster kidney decline.
Why Edema Happens in CKD
Your kidneys don’t just filter waste-they control how much water and salt stays in your blood. When kidney function drops below 60 mL/min/1.73m² (stage 3 CKD), they start losing their grip. Sodium builds up. Water follows sodium. And suddenly, fluid leaks out of your blood vessels and into your tissues. That’s edema. It doesn’t happen everywhere at once. Most often, it shows up in the lower legs because gravity pulls fluid down. But in advanced cases, you might see swelling around your eyes, in your belly (ascites), or even in your lungs. The real danger isn’t the puffiness-it’s what’s happening inside. Too much fluid means your heart has to work harder. Your blood pressure climbs. And your kidneys get even more stressed.Diuretics: The Fast Fix with Hidden Risks
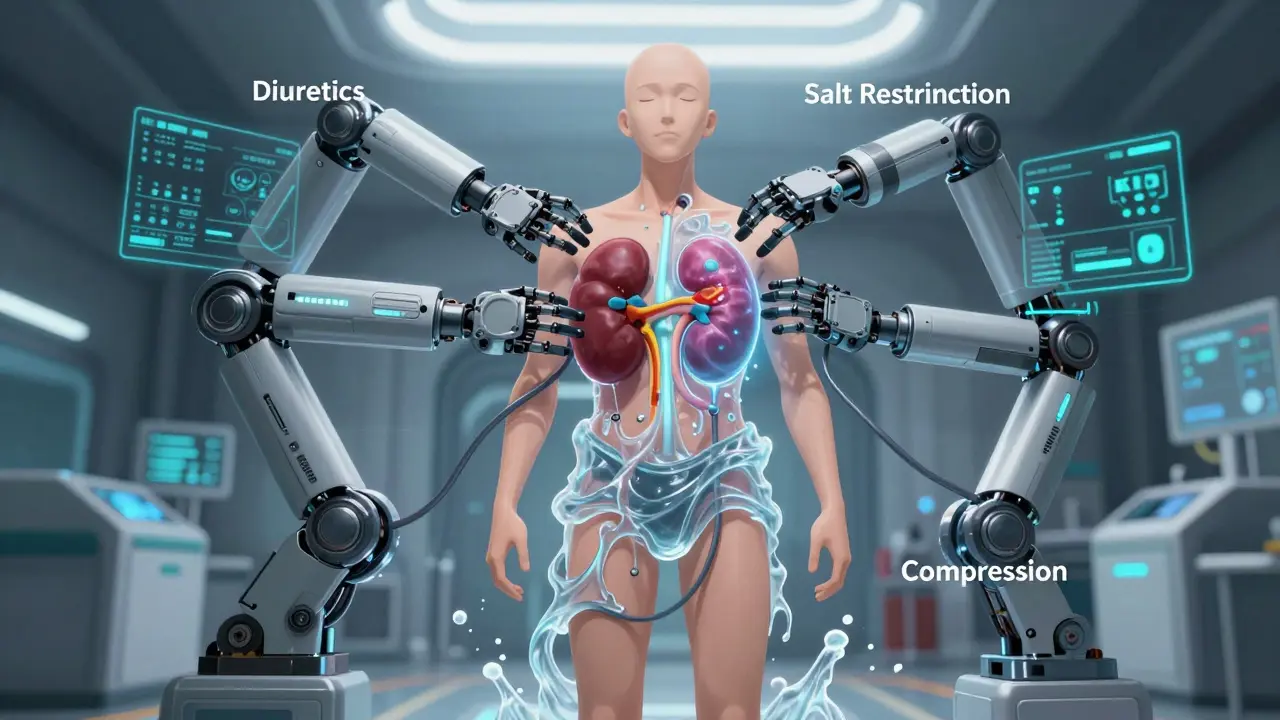
If you’ve been told to take a water pill, you’re not alone. Diuretics are the go-to tool for quickly draining excess fluid. But not all diuretics are the same-and not all are safe for every stage of CKD. For people with eGFR under 30, loop diuretics like furosemide, bumetanide, or torsemide are the standard. They work on the thick ascending limb of the loop of Henle, where most sodium gets reabsorbed. A typical starting dose is 40-80 mg of furosemide daily. If that doesn’t help, doctors may increase it by 20-40 mg every few days, sometimes up to 320 mg a day. But here’s the catch: the higher the dose, the riskier it gets. A 2016 NIH study found that people taking high-dose diuretics lost kidney function 3.2 mL/min/1.73m² per year-almost double the rate of those not on diuretics. And there’s a 47% higher chance they’ll need dialysis within a year. For those with milder CKD (eGFR above 30), thiazides like hydrochlorothiazide can still work. But when loop and thiazide diuretics are combined-called sequential nephron blockade-the fluid loss is stronger. That’s good for swelling. But it also raises the risk of sudden kidney injury by 23%. Spironolactone is another option, especially if you also have heart failure. It blocks aldosterone, which helps reduce fluid retention. But in late-stage CKD, it can spike potassium levels dangerously high-over 25% of patients with stage 4 or 5 CKD develop hyperkalemia on this drug. And now, there’s a new option: IV furosemide. Approved by the FDA in March 2025, it’s designed specifically for advanced CKD. In patients with eGFR under 15, it cleared 38% more fluid than oral pills. That’s huge. But it’s only for hospital or clinic use. You can’t take it at home.Salt Restriction: The Foundation No One Talks About
Here’s the truth most doctors don’t say out loud: diuretics won’t work well if you keep eating salty food. It’s like trying to bail out a boat with a hole in the bottom. The National Kidney Foundation recommends no more than 2,000 mg of sodium per day for anyone with CKD and edema. For stage 4 or 5, they suggest 1,500 mg. That’s less than one teaspoon of salt. But here’s the problem: 75% of sodium doesn’t come from your salt shaker. It’s hidden. - Two slices of bread: 300-400 mg sodium - One cup of canned soup: 800-1,200 mg - Two ounces of deli meat: 500-700 mg - One cup of yogurt: 100-150 mg - One cup of soup: 240 mL of fluid-yes, that counts too Most people don’t realize how fast sodium adds up. A single frozen meal can hit 1,500 mg. A bag of chips? 300 mg. A bottle of sports drink? 110 mg. You don’t need to be a chef to cut sodium-you need to read labels. And you need to avoid anything that says “sodium,” “salt,” or “monosodium glutamate” in the first five ingredients. A 2022 review from the American Kidney Fund found that people who stuck to 2,000 mg/day saw a 30-40% reduction in swelling within just 2-4 weeks-even without diuretics. That’s powerful. But it’s hard. Sixty-eight percent of CKD patients on a forum said they struggled with taste, social meals, or just not knowing what to eat. Working with a renal dietitian makes a difference. Studies show that three to four structured sessions on label reading, cooking swaps, and hidden sodium sources improve adherence and outcomes.Compression Therapy: The Quiet Hero
While diuretics and diet fight fluid from the inside, compression works from the outside. It’s simple: squeeze the legs to push fluid back up. Graduated compression stockings (30-40 mmHg at the ankle) are the gold standard. They’re tightest at the foot and loosen as they go up. This mimics the natural push of your calf muscles. Studies using water displacement show they reduce leg volume by 15-20% in four weeks. But most people don’t wear them. A 2022 study found only 38% kept using them past three months. Why? They’re hard to put on. They itch. They feel hot. Some people feel embarrassed wearing them. Elevation helps too. Lying down with your legs raised above your heart for 20-30 minutes a few times a day can reduce swelling by 25-30%. It’s free. It’s easy. And it works. For stubborn cases-especially with nephrotic syndrome-intermittent pneumatic compression devices can help. These machines inflate and deflate sleeves around your legs in cycles, pushing fluid upward. One study showed they reduced leg circumference 35% more than regular stockings. And movement? Walking 30 minutes five days a week improved edema control by 22% compared to just resting. Your calf muscles act like a second heart for your legs.The Balancing Act
There’s no single magic solution. Edema in CKD is managed by a team-nephrologist, dietitian, physical therapist, and you. Dr. David Wheeler from KDIGO says the window for diuretics in advanced CKD is narrow. Too much fluid? You risk heart failure. Too little? You risk kidney damage. The goal isn’t to drain every drop-it’s to reach your “dry weight,” the point where you’re not swollen but not dehydrated either. Dr. Ronald Falk reminds us: untreated fluid overload increases death risk by 28%. So sometimes, the risk of diuretics is worth it. The key is personalization. Someone with stage 3 CKD might control swelling with diet and walking alone. Someone with stage 5 may need IV diuretics, strict salt limits, and compression stockings every day.
What Works in Real Life
At the Mayo Clinic’s patient registry, those who got coordinated care-nephrologist, dietitian, and physical therapist-had a 75% success rate in controlling edema within eight weeks. Those on standard care? Only 45%. Real success means:- Waking up without puffy eyes
- Being able to tie your shoes
- Not needing to rush to the bathroom every hour
- Not feeling dizzy when you stand up
What’s Coming Next
Research is moving fast. The NIH’s FOCUS trial, due to finish in late 2025, is testing whether using bioimpedance (a quick, painless scan that measures body fluid) to guide diuretic doses reduces hospital visits. Early results show a 32% drop. New drugs like vaptans-designed to block water retention-were promising. But a 2024 trial was stopped because of liver damage. So for now, the old tools still win. The next KDIGO guidelines, expected in 2025, may shift toward slower, gentler fluid removal. Instead of chasing rapid weight loss, they may focus on steady, safe reduction to protect the kidneys.What You Can Do Today
Start with three simple steps:- Track your sodium. Use an app or a notebook. Write down everything you eat and drink for three days.
- Get compression stockings. Ask your doctor for a prescription for 30-40 mmHg graduated stockings. Try them for 10 days-don’t give up after one day.
- Walk. Even 15 minutes after dinner. Your legs will thank you.
Can I stop taking diuretics if I eat less salt?
Sometimes, yes-but only under medical supervision. In early-stage CKD, strict salt restriction can reduce or even eliminate the need for diuretics. But in advanced stages, your kidneys may not respond enough, even with perfect diet control. Never stop or change your dose without talking to your doctor. Stopping suddenly can cause fluid to rebound faster than before.
Why do my legs swell more at night?
Gravity pulls fluid down during the day as you stand and walk. At night, when you lie down, the fluid doesn’t drain as easily because your legs are level with your heart. That’s why swelling is often worse in the morning. Elevating your legs for 20-30 minutes before bed can help reduce overnight buildup.
Are compression stockings uncomfortable? Do they really work?
They can feel tight, especially at first. But 30-40 mmHg graduated stockings are designed to be firmest at the ankle and gradually looser up the leg-this helps push fluid upward. Studies show they reduce leg volume by 15-20% in four weeks. If they’re too painful, ask your doctor about different brands or sizes. Some have silicone bands or open toes for comfort. Don’t give up-consistent use matters more than perfection.
Can I drink as much water as I want if I’m on diuretics?
No. In advanced CKD, fluid intake is often limited to 1,500-2,000 mL per day-not just from drinks, but from foods too. Yogurt, soup, fruits like watermelon, and even ice cream count. Diuretics make you pee more, but if you keep drinking too much, your body just fills right back up. Your doctor will give you a daily fluid limit based on your weight, urine output, and kidney function.
Is it safe to use over-the-counter salt substitutes?
Most salt substitutes replace sodium chloride with potassium chloride. That sounds good-until you have CKD. Your kidneys can’t clear extra potassium well. High potassium levels can cause dangerous heart rhythms. Avoid potassium-based salt substitutes unless your doctor specifically says it’s safe. Use herbs, lemon juice, or vinegar instead.
Nicholas Urmaza
January 15, 2026 AT 07:37Let me tell you something straight - if you’re not tracking your sodium like it’s your job, you’re already losing. I’ve seen patients go from swollen ankles to tying their shoes again in under a month just by cutting out processed food. No magic pills. No fancy scans. Just reading labels. You want results? Stop blaming the diuretics and start blaming the frozen pizza.
And compression stockings? Yeah, they’re a pain to put on. But so is being hospitalized. Wear them. Or don’t. But don’t act surprised when your legs turn into water balloons.
This isn’t about being perfect. It’s about being consistent. One less bag of chips a day. One more walk after dinner. That’s how you win.
Sohan Jindal
January 16, 2026 AT 22:03They don’t want you to know this but the government and big pharma are pushing diuretics because they make billions. The real fix? Stop eating the poison they call food. Salt is a tool of control. They pump it into everything so you stay sick and keep buying meds. Why do you think your kidneys fail? It’s not age. It’s the system.
And compression socks? That’s just another scam. Your body knows how to heal itself if you stop poisoning it. Eat real food. Drink clean water. Walk barefoot. That’s the truth they don’t want you to hear.
Mike Berrange
January 18, 2026 AT 12:29Interesting that you mention the NIH study showing accelerated kidney decline with high-dose diuretics, yet you don’t address the fact that fluid overload carries a 28% higher mortality risk. That’s not a trade-off - that’s a damn cliff.
And you say ‘dry weight’ is the goal, but you never define it. What’s the clinical threshold? Is it 1 kg loss? 2? How do you measure it without bioimpedance? You’re giving advice without the tools to execute it.
Also - ‘don’t stop diuretics suddenly’ - why? What’s the pathophysiology behind rebound edema? You skip the science, so the reader is left guessing. That’s not education. That’s half-baked instruction.
Ayush Pareek
January 19, 2026 AT 20:40Hey, I’ve been living with CKD for 7 years now. I started with swelling so bad I couldn’t walk to the mailbox. I didn’t know where to begin.
What helped me most? Walking after dinner. Just 15 minutes. My legs didn’t feel like lead bricks anymore. And I swapped canned soup for homemade broth with herbs - no salt, just garlic and ginger.
Compression socks? I hated them at first. But I wore them while watching TV. Now I forget I’m wearing them. It’s not about being perfect. It’s about showing up.
You’re not alone. We’re all learning. One step at a time.
Nishant Garg
January 21, 2026 AT 17:53Let me tell you about my uncle in Delhi - he had stage 4 CKD, didn’t speak English, never read a label, but he ate like his ancestors did: dal, roti, seasonal veggies, no processed junk. No diuretics. No socks. Just walking to the temple every morning, squatting to wash his hands in the well, eating with his hands, no salt shaker in sight.
He’s 78 now. Swelling? Barely there. He doesn’t know what eGFR is. But his body knows what balance feels like.
Maybe the answer isn’t in the lab reports. Maybe it’s in the rhythm of old ways - slow food, quiet movement, community meals, no rush. We lost that. And now we’re paying for it with swollen ankles and hospital bills.
Not saying ditch science. But don’t forget wisdom that lived before the pill bottle.
Crystel Ann
January 23, 2026 AT 11:28I just started wearing the compression stockings after reading this. I was skeptical. But I put them on last night before bed and woke up with less puffiness around my ankles. It’s small, but it’s something.
I’m not trying to be perfect. I’m just trying to feel better. And for now, that’s enough.
Diane Hendriks
January 23, 2026 AT 12:21There’s a reason the West is drowning in chronic illness - we’ve outsourced responsibility to doctors and pills. We think medicine is a fix, not a bandage. But the real cure? Discipline. Sacrifice. Personal accountability.
Reading labels? Walking? That’s not healthcare. That’s character. And character is dying in this country. You want to beat edema? Stop looking for shortcuts. Start looking in the mirror.
ellen adamina
January 23, 2026 AT 22:47I’ve been tracking my sodium for two weeks. I didn’t realize how much was in yogurt. Or bread. Or the ‘low sodium’ soup I bought because it said ‘low’ on the front.
Turns out, ‘low’ is a lie. And I’m not mad. I’m just… aware now.
Thanks for the list. I’m printing it.
Tom Doan
January 25, 2026 AT 06:25So let me get this straight - we’re being told to wear compression socks, walk 30 minutes, read labels, and avoid salt substitutes… while being prescribed diuretics that might accelerate kidney failure?
Wow. What a beautifully coordinated medical circus.
At least we’re honest about the fact that we’re just managing symptoms while pretending we’re curing disease. Bravo. Applause.
Arjun Seth
January 26, 2026 AT 08:48You people are so lost. You think reading labels is the answer? You think walking helps? You think socks fix kidneys? NO. You need to understand - the body is a temple. And you are defiling it with your processed garbage, your lazy habits, your addiction to convenience. You want to live? Then change. Not tweak. Not adjust. CHANGE. Your kidneys are screaming. Are you listening? Or are you still scrolling through memes while your legs swell like balloons?
Stop blaming the system. Start blaming yourself. That’s the only path to healing. And if you can’t do it? Then you don’t deserve to live anyway.
And for God’s sake - stop drinking water like it’s a competition. Your kidneys are not a water filter. They’re a sacred organ. Treat them like one.