 Nov, 19 2025
Nov, 19 2025
Why Digoxin Can Be Dangerous If You Don’t Know These Interactions
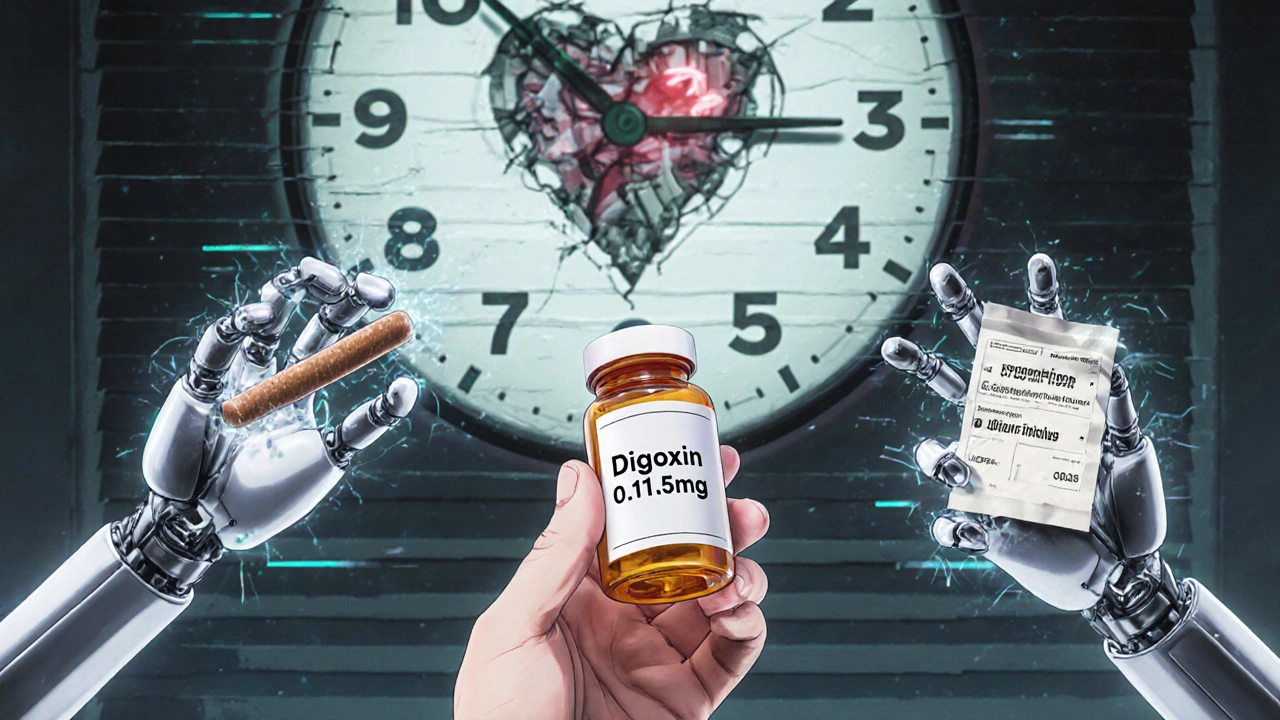
Digoxin has been used for over 90 years to treat heart failure and irregular heartbeats like atrial fibrillation. It’s cheap, effective, and still prescribed to millions - especially older adults. But here’s the problem: digoxin has a razor-thin safety margin. Too little, and it doesn’t work. Too much, and it can stop your heart. And the biggest danger isn’t the drug itself - it’s what you take with it.
What Digoxin Does (and Why It’s So Tricky)
Digoxin works by slowing down your heart’s electrical signals and making each beat stronger. It’s not a cure, but it helps you breathe easier and reduces hospital visits. The sweet spot for effectiveness is a blood level between 0.5 and 0.9 nanograms per milliliter. Once it hits 2.0, you’re in danger zone. Toxicity can happen even at normal levels if you’re over 65, underweight, or have kidney trouble. About 1 in 25 people on digoxin will have a toxic reaction - and many don’t see it coming until it’s too late.
The Top 5 Drug Interactions That Can Kill You
Some medications make digoxin stick around in your body longer. Others make it less effective. Either way, the results can be deadly.
- Dronedarone (Multaq): Used for atrial fibrillation, this drug can spike digoxin levels by over 50%. The 2012 PALLAS trial showed patients on both drugs had 2.5 times the risk of sudden death. If you’re on both, your digoxin dose must be cut in half - immediately.
- Verapamil and Diltiazem (Calan, Cardizem): These calcium channel blockers slow your heart rate. Combined with digoxin, your pulse can drop below 40 beats per minute. That’s not just slow - it’s life-threatening. Many patients end up needing a pacemaker.
- Amiodarone (Cordarone): This powerful antiarrhythmic can raise digoxin levels by up to 100%. One patient on Reddit reported his digoxin level jumped from 0.8 to 1.9 ng/mL after starting amiodarone. He ended up in the ER with blurred vision and vomiting.
- Quinidine: An older antiarrhythmic, still used in some cases. It cuts how fast your kidneys clear digoxin, causing dangerous buildup. Even small doses can trigger toxicity.
- Rifampin: An antibiotic used for TB and infections. It speeds up how fast your body breaks down digoxin - so your levels crash. You might think your medication isn’t working, but it’s just being flushed out too fast.
What You Eat and Drink Can Change How Digoxin Works
It’s not just pills. Your breakfast, snacks, and even herbal teas can mess with digoxin.
- Black licorice: Yes, really. The compound glycyrrhizin in black licorice pulls potassium out of your body. Low potassium + digoxin = high risk of dangerous heart rhythms. One study showed patients who ate just 100g of black licorice daily for two weeks developed arrhythmias while on digoxin.
- Oatmeal, high-fiber cereals, and milk: These can reduce digoxin absorption by 20-30%. If you take digoxin with your morning bowl of oatmeal, you’re getting less than half the dose you think you are. The fix? Take digoxin at least two hours before or after eating.
- Psyllium fiber supplements (Metamucil): These can cut digoxin absorption by 30-40% if taken within two hours. Many older patients take fiber for constipation - unaware it’s sabotaging their heart meds.
- St. John’s wort: This popular herbal remedy for depression activates a liver enzyme that clears digoxin from your body. One study showed levels dropped 25% after just one week. Your heart failure could get worse without you realizing why.
- Hawthorn: Often sold as a supplement for heart health, hawthorn can add to digoxin’s effect on heart rhythm - increasing the risk of dangerous QT prolongation.
Diuretics and Potassium: The Silent Killer Combo
Most heart failure patients take diuretics - water pills like furosemide (Lasix) or hydrochlorothiazide. These help reduce swelling and shortness of breath. But they also drain potassium from your body. Low potassium makes digoxin way more toxic. Even a slight dip - below 3.5 mmol/L - can turn a safe dose into a poison.
Doctors should check your potassium every month. If it’s low, they may switch you to a potassium-sparing diuretic like spironolactone. Don’t self-treat with potassium supplements - too much can also cause heart rhythm problems. Let your doctor guide you.
Who’s at Highest Risk?
Not everyone on digoxin is equally vulnerable. These factors raise your risk of toxicity:
- Age over 75
- Weight under 60 kg (132 lbs)
- Cracked kidneys (creatinine clearance under 50 mL/min)
- Already have heart block or slow heart rhythm
- Taking more than 0.25 mg per day
A 2023 risk score from the American College of Cardiology gives points for each of these. If you score 5 or higher, you need weekly blood tests - not every six months. That’s not routine. That’s urgent.
What to Do Right Now
If you’re on digoxin, here’s your action plan:
- Make a full list of every pill, supplement, and herbal product you take - including OTC antacids. Bring it to every appointment.
- Take digoxin at the same time every day - preferably on an empty stomach, two hours before or after meals.
- Avoid black licorice completely. Read labels on candy, tea, and chewing gum - it’s hiding in places you wouldn’t expect.
- Get your potassium checked monthly. If it’s below 3.5, tell your doctor immediately.
- If you start a new medication - even something for a cold or arthritis - ask: “Will this affect my digoxin?”
- Know the warning signs: nausea, vomiting, blurred vision, seeing yellow or green halos, or a pulse below 50. Call your doctor or go to the ER.
Why Digoxin Is Still Used - And When It’s Worth It
Digoxin prescriptions have dropped 38% since 2010. Newer drugs like SGLT2 inhibitors and ARNIs are safer and more effective. But digoxin still has a place. For older patients with persistent symptoms despite all the latest treatments, it can mean the difference between being bedridden and walking the dog. It’s not the first choice anymore - but for the right person, it’s still a lifeline.
The key? Monitoring. Blood tests. Knowing your interactions. And never assuming a new pill is harmless.
What Happens If You Miss a Dose or Take Too Much?
If you miss a dose, take it as soon as you remember - unless it’s close to your next dose. Never double up. If you accidentally take two doses, call your doctor or poison control. Don’t wait for symptoms.
If you overdose, you might feel dizzy, nauseous, or see strange colors. Your heart may race or slow down. Emergency treatment includes activated charcoal, IV fluids, and sometimes digoxin-specific antibodies - which can reverse toxicity in hours. But prevention is far better.
Can I take antacids with digoxin?
No - not at the same time. Antacids with aluminum or magnesium can reduce digoxin absorption by up to 30%. Take digoxin at least two hours before or after any antacid. Many ER visits for digoxin toxicity are linked to patients taking heartburn meds without knowing the risk.
Is digoxin safe for people with kidney problems?
It can be, but only with strict monitoring. If your creatinine clearance is below 50 mL/min, your dose must be lowered. Below 15 mL/min, many European guidelines advise against using digoxin at all. Kidneys clear digoxin - if they’re weak, the drug builds up. Always get your kidney function checked every 3-6 months.
Why do I need blood tests if I feel fine?
Because digoxin toxicity doesn’t always cause obvious symptoms at first. Many patients feel okay until they suddenly develop dangerous heart rhythms. Blood tests catch rising levels before you feel sick. If you’re on interacting drugs, you need testing every week - not every six months.
Can I take St. John’s wort for depression while on digoxin?
No. St. John’s wort makes your body clear digoxin 25% faster. That means your heart failure symptoms can return - and you won’t know why. Talk to your doctor about safer antidepressants like sertraline or citalopram. Don’t risk your heart for a supplement.
What should I do if I start a new heart medication?
Ask your cardiologist or pharmacist: “Will this change my digoxin level?” If it’s dronedarone, amiodarone, verapamil, or diltiazem - your digoxin dose will likely need to be cut in half. Never adjust your dose yourself. Even if you feel fine, your blood level could be climbing.
Are there any foods I should avoid besides licorice?
Yes. High-fiber foods like oatmeal, bran, and psyllium supplements can reduce digoxin absorption by 20-40%. Take digoxin two hours before eating. Also avoid large amounts of milk with your dose - it can interfere too. Stick to water when you take your pill.
How often should I get my digoxin level checked?
If you’re stable and not on interacting drugs, every 6 months is fine. But if you start a new medication, change your dose, or have kidney issues, check weekly for at least two weeks. The American College of Cardiology now recommends weekly testing for high-risk patients - and many doctors still aren’t doing it.
Final Advice: Don’t Guess. Test.
Digoxin isn’t a drug you can manage on autopilot. It’s not like blood pressure pills where you take it and forget it. Every new medicine, every dietary change, every shift in your kidneys - they all matter. Keep a log of what you take, when you take it, and how you feel. Bring it to every appointment. If your doctor doesn’t check your levels regularly, ask why. Your heart can’t afford a guesswork approach.
Liam Strachan
November 20, 2025 AT 17:38Michael Fessler
November 22, 2025 AT 04:04daniel lopez
November 22, 2025 AT 10:54Nosipho Mbambo
November 23, 2025 AT 23:30Katie Magnus
November 25, 2025 AT 15:21King Over
November 26, 2025 AT 21:30Johannah Lavin
November 27, 2025 AT 10:47Matthew Karrs
November 28, 2025 AT 21:13Destiny Annamaria
November 29, 2025 AT 23:22Ron and Gill Day
November 30, 2025 AT 09:12Gerald Cheruiyot
December 1, 2025 AT 15:36