 Jan, 13 2026
Jan, 13 2026
Cost-Benefit Medication Calculator
Evaluate Your Treatment Options
This tool helps you assess whether an expensive medication might be worth it for your situation, based on clinical effectiveness, side effects, and financial considerations.
Your Assessment Result
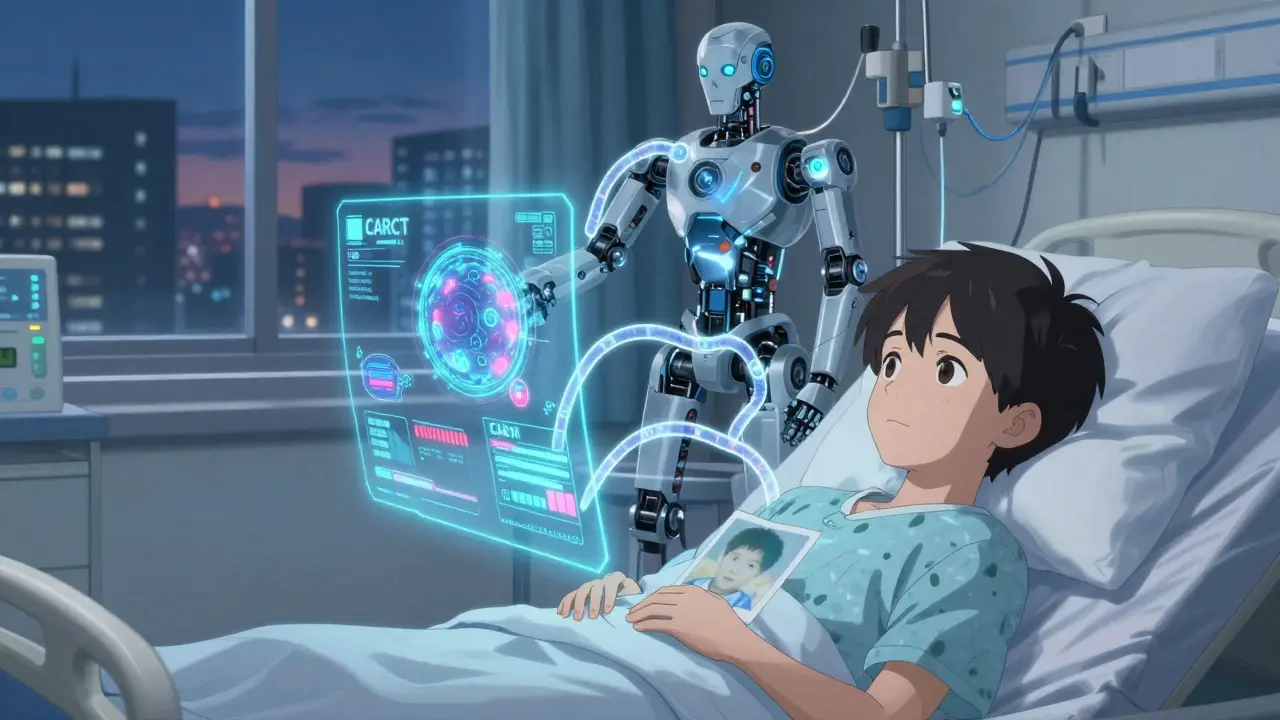
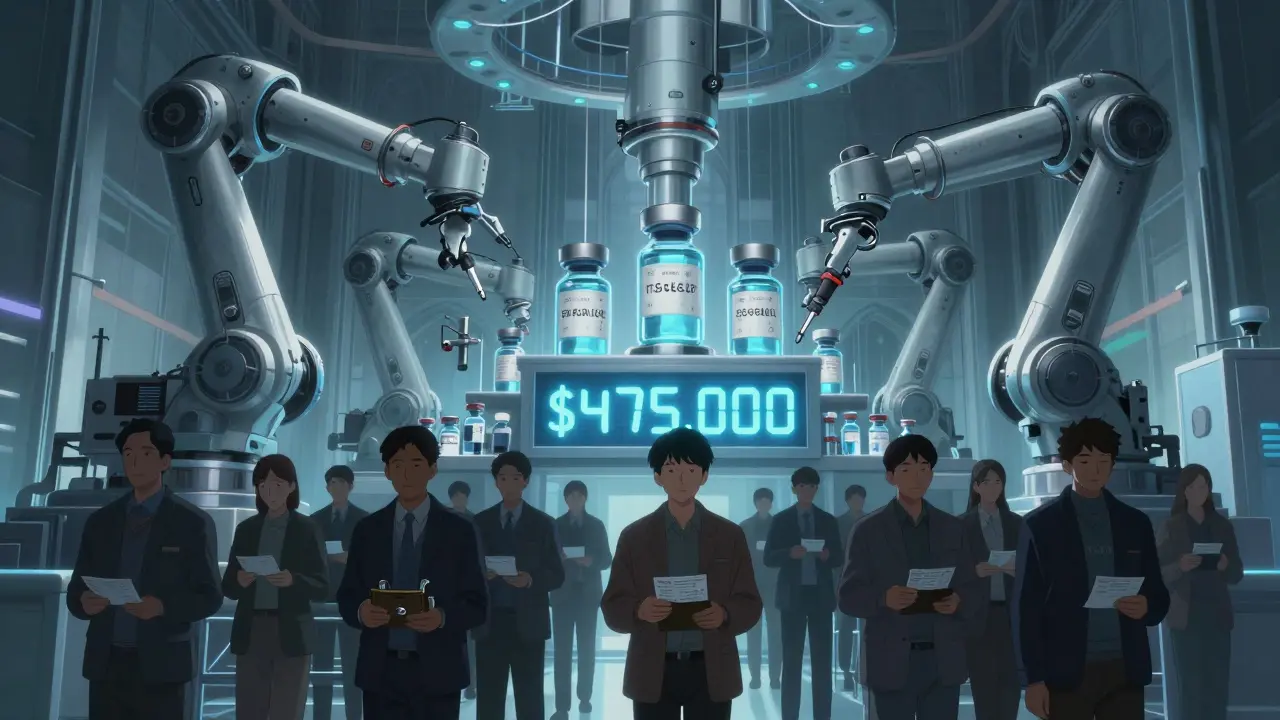
It’s 2026, and you’re staring at a $475,000 bill for a single cancer treatment. Your doctor says it could wipe out your tumors. But it also means weeks in the hospital, fever spikes, and a 30% chance of life-threatening inflammation. You’ve already spent $12,000 out of pocket this year. You’re not sure you can afford it. But you’re also not sure you can afford not to.
This isn’t a hypothetical. It’s real life for tens of thousands of Americans every year. And the question isn’t just about money-it’s about what value means when your life is on the line.
Why Some Drugs Cost More Than a House
The most expensive drugs today aren’t just pricey because of research. They’re priced that way because they’re built for tiny groups of people. Think gene therapies for rare genetic disorders, CAR-T cell treatments for advanced leukemia, or biologics for autoimmune diseases that don’t respond to anything else. These aren’t mass-market pills. They’re custom-made biological machines, often requiring years of development and specialized manufacturing.
In 2024, the median cost of the 50 most expensive drugs covered by Medicare hit $16,178 per dose. Thirty-one of them were biologics. Sixteen were small molecules. Three were gene therapies. And 72% of those top drugs were approved for rare diseases under the Orphan Drug Act-a law meant to encourage innovation for conditions affecting fewer than 200,000 Americans. That’s why a single shot of a drug for a rare blood disorder can cost more than your car payment for a year.
But here’s the twist: many of these drugs don’t work for everyone. A 2024 study found that 56% of the most expensive drugs had low or moderate therapeutic benefit according to European health agencies. So why are they still being prescribed? Because for the small group they do help, they’re life-changing.
When Side Effects Are Worth It
Every medication has side effects. Even aspirin can cause stomach bleeding. But with ultra-expensive drugs, the side effects are often severe: cytokine release syndrome, organ damage, prolonged hospital stays, or even secondary cancers. So when does it make sense to accept that risk?
Take tisagenlecleucel, a CAR-T therapy for children with relapsed acute lymphoblastic leukemia. It costs nearly half a million dollars. It requires a month-long hospital stay. It can cause seizures, low blood pressure, and brain swelling. But for kids who’ve run out of chemo options, it offers a 70-80% chance of long-term remission. In one 2023 patient forum, 78% of families said the treatment was worth it-even with the trauma of the side effects.
Compare that to older treatments. Before CAR-T, these kids faced bone marrow transplants with 30-40% survival rates and lifelong immune suppression. The new drug isn’t perfect. But it’s better. And in medicine, “better” doesn’t always mean “safer.” Sometimes it means “more likely to save your life.”
Same goes for hepatitis C drugs like Harvoni. In 2016, a full course cost over $80,000. Out-of-pocket for many was $7,000. But it cured 95% of patients in 12 weeks. The old treatment? Interferon injections for a year, with flu-like symptoms, depression, and only a 50% cure rate. People chose the expensive drug because the alternative was worse-physically, emotionally, and financially.
Who Pays, and How Much?
Here’s the ugly truth: the person who needs the drug often pays the most.
In 2019, Medicare Part D beneficiaries without low-income subsidies paid 2.5 times more out of pocket than commercially insured patients for the same ultra-expensive drugs. One patient with hemophilia paid $15,000 a month for emicizumab. Another spent $5,692 just for ruxolitinib. And 68% of people taking drugs over $10,000 a month admitted to skipping doses because they couldn’t afford them. Forty-two percent said they chose between buying meds and buying food.
The system is broken. Medicare Part D has a coverage gap-the “donut hole”-where after you spend a certain amount, you pay 100% of the cost until you hit catastrophic coverage. In 2021, 2.3 million people got stuck there. And even when you hit catastrophic coverage, you still pay 5% of the drug’s list price. For a $100,000 drug, that’s $5,000 out of pocket. That’s not affordable. That’s a sentence.
Meanwhile, drugmakers say they need high prices to fund R&D. Tufts University estimated it costs $2.6 billion to bring a new drug to market. But independent analyses show that 32 out of 50 new drugs approved between 2017 and 2018 offered only marginal improvements over existing treatments. That’s not innovation. That’s incrementalism priced like a breakthrough.
The Real Value Isn’t in the Price Tag
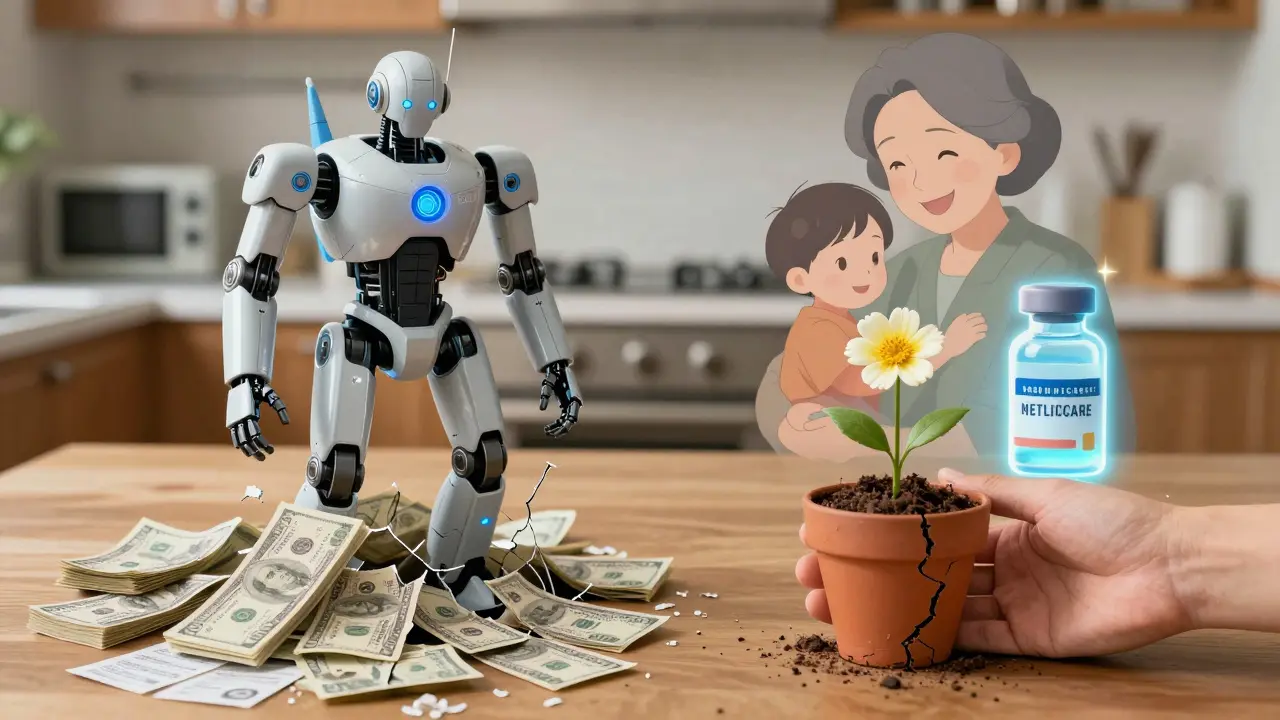
Value isn’t about how much a drug costs. It’s about what it buys you: time, mobility, independence, life.
Consider a patient with rheumatoid arthritis. She tried six cheaper drugs. None worked. Her joints were collapsing. She couldn’t hold her grandkids. Then she got a biologic that cost $20,000 a month. It gave her back her hands. She started gardening again. She took a trip to see her daughter in Oregon. The drug didn’t cure her. But it gave her quality of life. That’s worth more than money.
That’s the core of cost-benefit analysis. It’s not just about survival. It’s about living. The U.S. doesn’t have a formal threshold for what’s “worth it,” unlike the UK, which uses a cost-per-QALY (quality-adjusted life year) metric. If a drug costs more than $150,000 per QALY gained, it’s usually rejected. But in America, if a drug works-even if it’s expensive and risky-it often gets covered. Because we don’t have a price on life. We just have a price on the system.
How to Navigate the System
If you’re facing a high-cost drug, you’re not alone-and you don’t have to pay full price.
- Manufacturer patient assistance programs cover an average of 40% of out-of-pocket costs for commercially insured patients. Apply early-some require medical documentation and can take weeks.
- Independent foundations like the Chronic Disease Fund gave out $2.1 billion in aid in 2022. They help with copays for autoimmune, cancer, and rare disease drugs.
- Specialty pharmacies have case managers who spend 3+ hours per patient just navigating insurance. Ask your doctor to refer you.
- Medicare Part D has a cap on out-of-pocket spending starting in 2025. Before then, know your plan’s phases: deductible, initial coverage, donut hole, catastrophic. Don’t guess-use the Medicare Plan Finder tool.
- Ask about alternatives. Sometimes a different brand, a biosimilar, or even a lower-dose regimen can cut costs without losing efficacy.
And don’t be afraid to push back. Insurance companies deny 1 in 5 prior authorization requests. If your drug is denied, appeal. You have rights. And sometimes, just asking for a price reduction works. In 2016, NICE in the UK rejected daratumumab because it cost £120,000 per QALY. After the manufacturer dropped the price to £45,000, they approved it.
The Bigger Picture
By 2030, specialty drugs will make up 79% of all pharmacy spending in the U.S. That’s not sustainable. The Inflation Reduction Act of 2022 started Medicare drug price negotiations in 2024-but only 10 drugs qualify. 96% of the most expensive drugs are still off-limits.
But change is coming. In 2023, 82% of Americans said drug prices are unreasonable-even though most agreed drugs save lives. That’s the tension. We want miracles. We just don’t want to pay for them alone.
The future of healthcare isn’t just about making drugs cheaper. It’s about making value transparent. About linking price to real outcomes. About asking: Is this drug worth what it costs? And if it is, who should pay?
There’s no perfect answer. But there is a better question: When a drug gives you back your life, how much is that really worth?
Are expensive medications always worth the cost?
No. Many ultra-expensive drugs offer only marginal improvements over cheaper alternatives. Studies show that fewer than 15% of new drugs provide major therapeutic progress. But for a small group of patients with no other options-like those with advanced cancer, rare genetic disorders, or treatment-resistant autoimmune diseases-these drugs can be life-saving. The key is matching the drug to the patient’s specific needs, not just the price tag.
Why do some drugs cost so much more than others?
The cost reflects development complexity, manufacturing precision, and patient population size. Gene therapies and CAR-T treatments are custom-made for individuals, requiring lab-grown cells and specialized facilities. Drugs for rare diseases (orphan drugs) are priced high because the manufacturer must recoup costs from a tiny number of patients. Biologics, which are made from living cells, are also harder and more expensive to produce than traditional pills.
Can I get financial help to afford high-cost drugs?
Yes. Most drug manufacturers offer patient assistance programs that can cover 30-100% of out-of-pocket costs. Independent nonprofits like the Chronic Disease Fund and Patient Access Network Foundation provide grants. Specialty pharmacies often assign case managers to help navigate insurance. Medicare Part D also has a cap on out-of-pocket spending starting in 2025. Always ask your doctor or pharmacist about these options-don’t assume you’re on your own.
What if my insurance denies coverage for an expensive drug?
Denials are common, but they’re not final. You have the right to appeal. Start by asking for a written explanation of the denial. Then submit a formal appeal with supporting letters from your doctor, clinical trial data, and evidence of prior treatment failures. Many appeals succeed, especially if you can show the drug is medically necessary and alternatives have failed. Some patients also get help from patient advocacy groups that offer free legal advice.
Do side effects make expensive drugs less worth it?
It depends on the severity of the side effects versus the benefit. For example, CAR-T therapy can cause cytokine release syndrome, which requires ICU care. But for a patient with terminal leukemia, that risk may be worth it if it leads to remission. Similarly, hepatitis C drugs like Harvoni had high costs but eliminated the need for painful interferon injections and boosted cure rates from 50% to 95%. The trade-off isn’t just financial-it’s about quality of life. If the side effects are manageable and the outcome is transformative, many patients say yes.
Will drug prices come down in the future?
Slowly, and only for some. The Inflation Reduction Act allows Medicare to negotiate prices for 10 drugs starting in 2026-but 96% of the most expensive drugs are currently excluded. Biosimilars (cheaper versions of biologics) are starting to enter the market and could cut costs by 20-40%. But until there’s a national cost-effectiveness threshold-like the UK’s-prices will remain high for drugs that work, even if they’re not groundbreaking. The real shift will come when payers demand proof of real-world value before covering new drugs.
Priyanka Kumari
January 14, 2026 AT 12:38As someone who’s watched my aunt go through CAR-T therapy, I can say this: the cost isn’t the real issue-it’s the silence around it. No one tells you how lonely the hospital stays are, or how your kids start avoiding the word ‘cancer’ at school. But when she walked out of that hospital holding her grandson for the first time in a year? Worth every penny. We need more compassion in pricing, not just spreadsheets.
Also, shoutout to patient assistance programs-they saved us from bankruptcy. Ask for help. No shame in it.
Avneet Singh
January 15, 2026 AT 07:27Let’s be candid: the entire pharmaceutical industrial complex is a rent-seeking oligopoly masquerading as innovation. The marginal therapeutic gain of 82% of these ‘breakthrough’ biologics is statistically negligible-yet they command premium pricing due to regulatory capture and patent evergreening. The Orphan Drug Act, originally intended to incentivize neglected disease research, has been weaponized into a profit-maximization engine. We are not dealing with medicine. We are dealing with financial engineering dressed in lab coats.
Adam Vella
January 15, 2026 AT 18:56There is a fundamental philosophical tension here: the sanctity of life versus the economics of scarcity. In utilitarian terms, allocating $475,000 to one patient could fund hundreds of preventative care interventions. But in deontological ethics, each individual life possesses intrinsic, non-negotiable value. The American system, for all its flaws, leans toward the latter-because to assign a price to survival is to deny the dignity of personhood.
That said, the lack of cost-effectiveness thresholds is not a virtue-it is a moral failure masked as freedom.
vishnu priyanka
January 16, 2026 AT 04:48Man, I read this while sipping chai in Delhi, thinking about my cousin back home who can’t even afford insulin. This isn’t just an American problem-it’s a global joke. We got folks in rural India paying 10x more for generics because of middlemen and corruption. Meanwhile, some rich kid in Texas gets a $500K gene therapy and posts about it on Instagram like it’s a new Tesla.
Maybe the real question isn’t ‘is it worth it?’ but ‘why does anyone have to choose?’
Angel Tiestos lopez
January 18, 2026 AT 04:26Bro. I lost my mom to cancer. She took the expensive drug. Got sick as hell. Missed my graduation. But she lived long enough to see me get hired. So yeah, it was worth it. 🤍
Also, if you’re crying over a $5k copay, go talk to someone who’s paying $15k/month for a drug that doesn’t even work. That’s the real horror story. 🙏
Alan Lin
January 18, 2026 AT 14:40Let me be unequivocal: the current system is indefensible. The fact that a patient must choose between food and medication is not a market failure-it is a moral catastrophe. The pharmaceutical industry operates under a license to print money, shielded by patent monopolies and lobbying power that dwarfs public interest. The existence of patient assistance programs is not a solution-it is a Band-Aid on a severed artery.
We must implement a national cost-effectiveness framework, cap out-of-pocket expenditures at 5% of household income, and mandate transparency in R&D spending. Anything less is complicity in systemic violence against the sick.
Pankaj Singh
January 19, 2026 AT 11:41Everyone’s acting like these drugs are miracles. Newsflash: 56% of them have low therapeutic benefit. You’re not saving lives-you’re prolonging suffering while billing $200k per month. These companies aren’t curing disease. They’re selling hope on credit cards. And you’re all too busy crying about your copay to notice you’re being scammed.
Stop romanticizing financial ruin. This isn’t heroism. It’s exploitation.
Randall Little
January 20, 2026 AT 20:27So let me get this straight: we’re okay with a system where a child’s chance at life is determined by their parents’ credit score? And we call this capitalism? Interesting. In Sweden, they’d say that’s socialism. In China, they’d call it feudalism. In America? We call it ‘freedom.’
Meanwhile, the same companies that charge $500k for a drug spent $1.2 billion lobbying Congress last year. Coincidence? Or just the American way?
Acacia Hendrix
January 20, 2026 AT 22:10The QALY metric is not merely a tool-it is the only ethically coherent framework for resource allocation in healthcare. The U.S. refusal to adopt any form of cost-effectiveness analysis is not a reflection of values; it is an indictment of intellectual cowardice. The absence of thresholds enables rent extraction under the guise of compassion. This is not moral ambiguity-it is moral bankruptcy dressed in clinical jargon.
James Castner
January 21, 2026 AT 05:55Let’s pause for a moment and recognize the deeper truth beneath this crisis: we are not just debating drug pricing-we are confronting the existential question of what we owe each other as a society. When a parent chooses between insulin and groceries, they are not making a financial decision-they are performing an act of love under duress.
The pharmaceutical industry has weaponized hope. But hope without access is a cruel illusion. We must rebuild our healthcare system not as a market, but as a covenant-a sacred promise that no one will be abandoned because they cannot pay. This is not socialism. This is sanity. This is humanity.
And if we fail to act, we will one day look back and realize: we didn’t just let people die. We let them die while watching the stock price rise.
Adam Rivera
January 21, 2026 AT 13:44Hey, just wanted to say-this thread hit me hard. My sister’s on one of these drugs. She’s been on it for 18 months. She can’t work, but she’s alive. And she laughs again. That’s worth more than any number.
Also, if you’re struggling with costs, DM me. I’ve been through the paperwork hell. I can point you to the right foundations. You’re not alone.