 Dec, 1 2025
Dec, 1 2025
For millions of people taking multiple medications, the idea of a single pill that combines two or more drugs sounds like a dream. Fewer pills to remember. Simpler routines. But here’s the catch: that convenience often comes at a price - sometimes 10 times higher than buying the same drugs separately as generics.
Why Combo Pills Cost So Much
Fixed-dose combination (FDC) drugs pack two or more active ingredients into one tablet or capsule. Common examples include Janumet (sitagliptin + metformin) for diabetes, Entresto (sacubitril + valsartan) for heart failure, and Kazano (alogliptin + metformin). On the surface, they look efficient. But look closer, and the pricing doesn’t add up. In 2016, Medicare Part D spent $925 million more on 29 branded combo pills than it would have if patients had taken the same ingredients as separate generic drugs. That’s not a typo. $925 million. And that was just one year. Take Janumet. The branded combo cost Medicare about $472 for a 30-day supply. Meanwhile, generic metformin - one of the two ingredients - costs as little as $4 for the same amount at Walmart’s $4 generic program. The other ingredient, sitagliptin, was still under patent at the time, but even if you added the cost of the branded sitagliptin alone, you’d still pay less than the combo. Same story with Kazano: $425 a month for the combo, versus under $10 for generic metformin. The math is simple: 1 + 1 doesn’t equal 1. It often equals 1.6 - meaning branded combos cost about 60% of what two separate branded drugs would cost. But when one or both components are already generic? That 1.6 becomes 10 or even 15. That’s not innovation. That’s pricing.The Evergreening Trap
Pharmaceutical companies don’t just make combos to help patients. They make them to extend profits. When a drug’s patent is about to expire, manufacturers often pair it with another, already-generic drug to create a new combo product. This new combo gets its own patent, even though none of the ingredients are new. This tactic is called “evergreening.” It’s legal. And it’s profitable. Nexlizet, for example, combines ezetimibe (a generic cholesterol drug for over a decade) with bempedoic acid (a newer, patented drug). Even though ezetimibe costs pennies, Nexlizet sells for $12 a day in the U.S. That’s over $4,000 a year - while the generic ezetimibe alone costs less than $20. The FDA approves these combos because they’re technically new formulations. But the clinical benefit? Often minimal. The real benefit is financial.Who Pays the Difference?
You might think, “If I’m not on Medicare, why should I care?” But you do. Medicare’s spending affects drug prices for everyone. When Medicare pays more for a drug, private insurers follow suit. Pharmacies, PBMs (pharmacy benefit managers), and employers all adjust their pricing based on what the largest payer - Medicare - is willing to cover. And it’s not just Medicare. The Department of Veterans Affairs pays 22-33% less than Medicare for the exact same drugs. That means veterans get the same meds for far less. Meanwhile, millions of other Americans pay the higher price. The numbers don’t lie: combo drugs made up only 2.1% of all Part D prescriptions in 2021, but they accounted for 8.3% of total spending. That’s disproportionate. And it’s not because they’re more effective. It’s because they’re more expensive.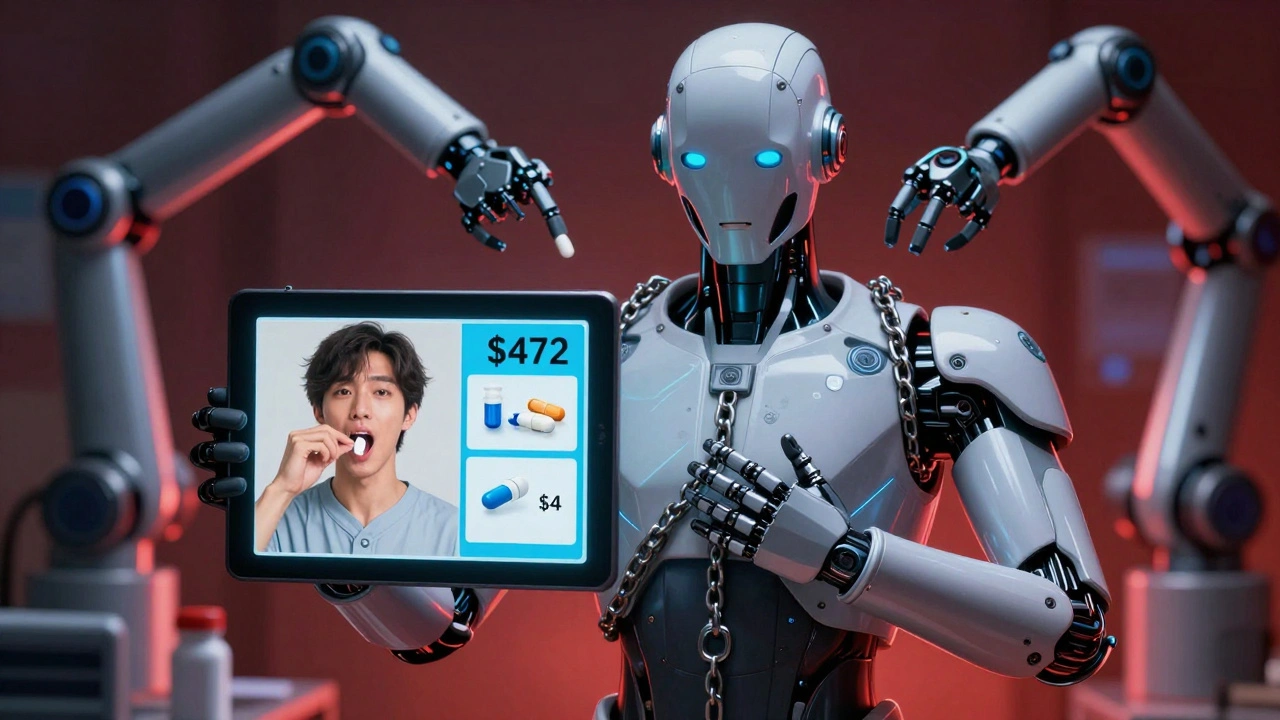
Why Doctors Still Prescribe Them
You might wonder: if the cost difference is so huge, why aren’t doctors pushing for generics? One reason: adherence. Studies show patients are 15-20% more likely to take their meds regularly when they’re in a single pill. For someone managing diabetes, high blood pressure, and cholesterol, juggling five different pills a day is overwhelming. A combo reduces that to two or three. That’s real. The American College of Cardiology found that for patients with multiple chronic conditions, combos improved adherence by up to 25%. That means fewer hospital visits, fewer complications, and lower long-term costs. But here’s the problem: that adherence benefit doesn’t justify a $400-a-month pill when you could get the same effect for $30. The question isn’t whether combos help people take their meds. It’s whether we’re paying too much for that help.What You Can Do
If you’re on a combo drug, ask your doctor or pharmacist:- Are the individual components available as generics?
- What’s the total cost if I buy them separately?
- Can I split the dose safely? (Some combos can be split - like taking one generic metformin and one generic valsartan - if the doses match.)
- Is there a patient assistance program for the combo? Some manufacturers offer co-pay cards - but these rarely bring the price down to generic levels.
The Bigger Picture
The Inflation Reduction Act of 2022 gave Medicare the power to negotiate drug prices for the first time. That could eventually bring down combo prices - but only for a small number of high-cost drugs. And it won’t apply to most people until 2026. Meanwhile, the FDA is pushing to speed up generic approvals. More generic competition means lower prices for individual components - which should, in theory, make combos less profitable. But manufacturers are already adapting. They’re developing new combos with newer, non-generic ingredients - and pricing them even higher. The real solution? Transparency. Patients need to know the true cost of their meds. Pharmacies need to flag when a combo is dramatically more expensive than generics. Doctors need to have the conversation - not just prescribe the easiest option.Is There a Better Way?
Some health systems are already trying. The University of Michigan Health System found that by reviewing combo prescriptions quarterly and switching patients to separate generics when possible, they saved an average of $1,200 per patient per year. That’s not just savings. That’s better care. When patients pay less, they’re more likely to stick with their treatment. When they don’t have to choose between medicine and groceries, their health improves. The future of drug pricing isn’t about more combos. It’s about smarter choices. It’s about letting patients and doctors pick what works - not what’s most profitable.Combination pills aren’t bad. But when you’re paying ten times more for the same medicine - just because it’s packed into one tablet - that’s not convenience. That’s a system that’s broken.
ATUL BHARDWAJ
December 2, 2025 AT 02:33India also has this problem but we call it 'combo pack' and pharmacies sell it cheaper. Still, doctors push branded ones because of kickbacks. Simple math: 1+1=10 here. Sad.
Rebecca M.
December 2, 2025 AT 07:21Oh wow, so the pharma companies didn’t just invent the combo pill - they invented the ‘pay-more-for-less’ pill. Genius. I’m filing for a patent on breathing air next.
Lynn Steiner
December 3, 2025 AT 00:26I cried when I saw my bill. $425 for a pill that should cost $10. I’m not even mad anymore. I’m just… empty. 💔
Alicia Marks
December 4, 2025 AT 22:41You got this. Ask your doc about generics. It’s not hard, and it could save you hundreds. You deserve to feel better without going broke.
Joel Deang
December 5, 2025 AT 19:08bro i just found out my janumet costs 5x more than metformin alone and i thought i was being smart buying the combo… turns out i was just being scammed. lmao. pharmacy said they can split it tho. gonna try it next month 🤞
dave nevogt
December 7, 2025 AT 09:01This isn’t just a pricing issue - it’s a systemic betrayal of trust. We’ve allowed the medical-industrial complex to reframe convenience as necessity, and then monetize our dependency. The pill isn’t the problem; the narrative is. We’ve been conditioned to believe that fewer pills = better care, when in reality, it’s fewer bills = better care. The real innovation would be transparency, not formulation. But innovation is a luxury when profit is the only metric that matters.
Arun kumar
December 7, 2025 AT 14:29in india we have this too but we call it 'combo pack' and it's usually cheaper cause generics are everywhere. but doctors still push branded combos for commission. same game. sad but true.
Zed theMartian
December 7, 2025 AT 23:40Oh please. The real villain here is the average American who’d rather pay $400 for a ‘convenient’ pill than spend 30 seconds opening two blister packs. You want lower prices? Stop being lazy. The market rewards apathy.
Ella van Rij
December 8, 2025 AT 21:59Ohhh so that’s why my PBM ‘negotiated’ my combo down to $380… instead of $420. My bad for thinking they were on my side. 😘
Steve World Shopping
December 9, 2025 AT 22:18The structural inefficiencies in pharmaceutical supply chains are exacerbated by regulatory arbitrage and patent thickets. The FDC model represents a suboptimal equilibrium in the principal-agent dynamic between prescribers and patients, wherein informational asymmetry enables rent-seeking behavior. Bottom line: this is rent extraction disguised as innovation.
Paul Keller
December 10, 2025 AT 06:48Look, I get the cost argument. But if you’re 72, diabetic, hypertensive, and taking five pills a day, the mental load is real. I’ve seen patients forget meds, end up in the ER, and it costs the system way more than the combo. Convenience isn’t just about pills - it’s about dignity. The problem isn’t the combo. It’s that we let the system make dignity a luxury.
Shannara Jenkins
December 10, 2025 AT 16:01My mom switched from Entresto to separate generics and now pays $28/month. She was scared at first, but her pharmacist walked her through it. She’s doing great. You can do this too - it’s not scary, just smart.
Elizabeth Grace
December 12, 2025 AT 02:04OMG I just checked my script - Janumet was $410. I Googled metformin and sitagliptin separately… $38 total. I’m going to scream. I’m going to cry. I’m going to call my doctor tomorrow. This is insane.