 Dec, 29 2025
Dec, 29 2025
Drug Interaction Risk Calculator
How Dangerous Is This Combination?
This tool estimates your risk of dangerous low blood pressure based on your medications and health factors. Based on studies showing a 5.3x higher risk of hospitalization when combining clarithromycin with calcium channel blockers.
Please select your medications and health factors to see your risk level.
When you’re prescribed clarithromycin for a stubborn chest infection, you probably don’t think about your blood pressure meds. But if you’re also taking a calcium channel blocker like nifedipine or amlodipine, this combo can drop your blood pressure so low you end up in the hospital - sometimes even in intensive care.
What’s Really Going On Between These Two Drugs?
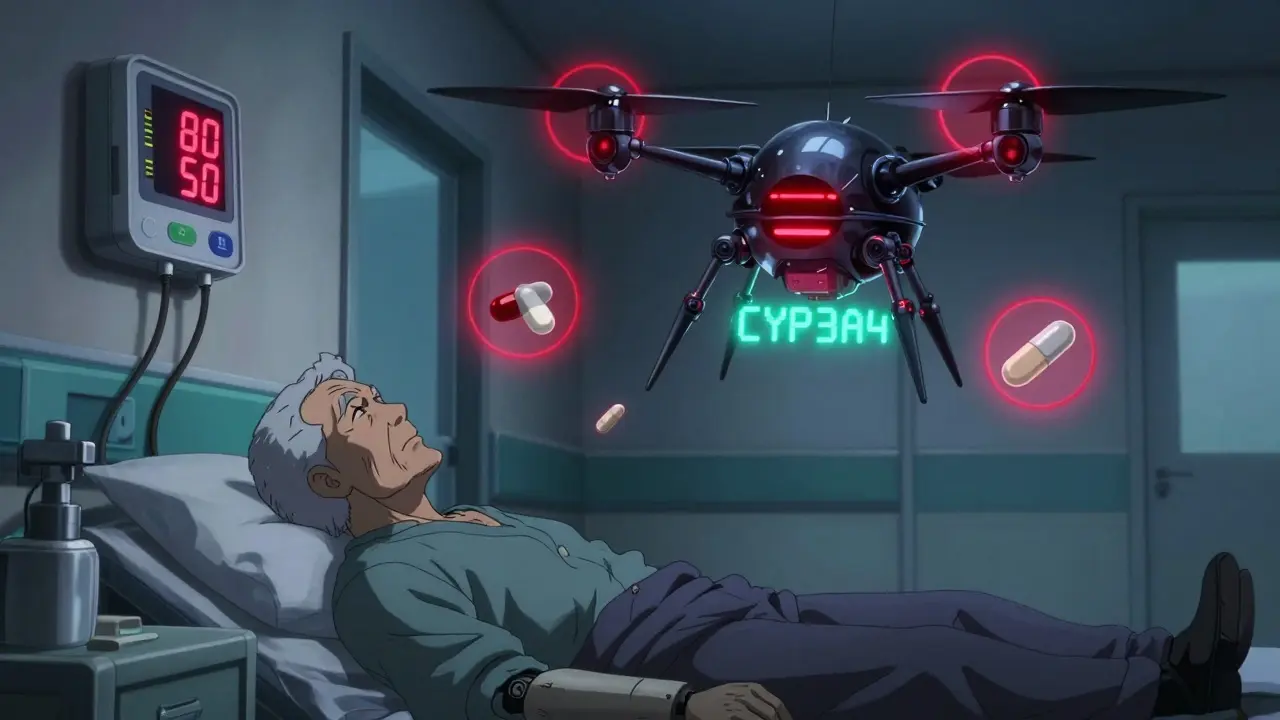
Clarithromycin doesn’t just kill bacteria. It also shuts down a key enzyme in your liver called CYP3A4. This enzyme is responsible for breaking down most calcium channel blockers, especially the dihydropyridines like nifedipine, amlodipine, and felodipine. When clarithromycin blocks this enzyme, your body can’t clear the blood pressure medication properly. The result? The drug builds up in your bloodstream, sometimes doubling or even tripling its concentration. That’s not theoretical. A 2013 study tracking over 96,000 people found that those taking clarithromycin along with a calcium channel blocker had a 5.3 times higher risk of dangerous drops in blood pressure compared to those taking azithromycin - another antibiotic that doesn’t interfere with CYP3A4. One patient in the study went from a normal blood pressure of 130/80 to 80/50 in just 48 hours. His heart rate dropped. His kidneys started to fail. He needed IV fluids and ICU monitoring.Not All Calcium Channel Blockers Are Equal
The risk isn’t the same across the board. Nifedipine is the most dangerous combo with clarithromycin. Studies show it has the highest odds ratio - over five times more likely to cause severe hypotension than other CCBs. Felodipine and nicardipine are next in line. Amlodipine is more commonly prescribed, so it shows up more often in cases, but it’s slightly less risky than nifedipine. Verapamil and diltiazem are non-dihydropyridines. They’re still risky, but for different reasons. They affect heart rhythm as well as blood pressure. Add clarithromycin, and you can get not just low blood pressure, but also a dangerously slow heart rate. One 72-year-old man on amlodipine and clarithromycin developed a heart rate of 48 beats per minute and collapsed. He had to be hospitalized.Why Azithromycin Is the Safer Choice
Here’s the good news: there’s a simple fix. Switch to azithromycin. Unlike clarithromycin, azithromycin doesn’t inhibit CYP3A4. The same 2013 JAMA study showed no increased risk of hospitalization or kidney injury when azithromycin was used instead. In fact, replacing clarithromycin with azithromycin cuts the risk of bad outcomes by half. Despite this, a 2016 study found that nearly 13% of clarithromycin prescriptions in people over 65 were still being written to patients on CCBs. Why? Because many prescribers aren’t trained to catch this interaction. Electronic health records often don’t flag it. And clarithromycin is cheaper than azithromycin in some places - a false economy when you consider the cost of an ICU stay.
Who’s at the Highest Risk?
Older adults. People with kidney problems. Those already on multiple blood pressure meds. If your eGFR (a measure of kidney function) is below 60, your body clears drugs slower. That means even a small increase in calcium channel blocker levels can push you over the edge. Add a beta-blocker like metoprolol? That’s another layer of risk. Beta-blockers slow your heart rate. Calcium channel blockers do too. Together with clarithromycin, you’re setting up a perfect storm: low blood pressure, low heart rate, low cardiac output. The result? Dizziness, fainting, falls, acute kidney injury - and sometimes death.Real Cases, Real Consequences
A 76-year-old woman in Canada was prescribed clarithromycin for bronchitis. She’d been on nifedipine for 10 years. Within two days, her blood pressure crashed. Her kidneys shut down. She spent a week in hospital. Her doctor later said, “I didn’t think about the interaction. I thought it was just a chest infection.” In the U.S., the FDA’s adverse event database recorded over 1,800 cases of hypotension linked to this combo between 2010 and 2020. The reporting odds ratio was nearly four times higher than other antibiotic-CCB pairs. That’s not noise - that’s a signal.What Doctors Should Do - And What You Should Ask
If you’re prescribed clarithromycin and take a calcium channel blocker:- Ask: “Is there a safer antibiotic I can use instead?”
- Ask: “Could this interact with my blood pressure medicine?”
- If you’re over 65 or have kidney disease, insist on azithromycin.
- Never prescribe clarithromycin to someone on nifedipine.
- Check your EHR system - does it flag this interaction? If not, manually review all CCB prescriptions before writing macrolides.
- Monitor blood pressure every 4-6 hours for the first 72 hours if you must use clarithromycin - and only if no alternative exists.
- Discontinue clarithromycin immediately if systolic BP drops below 90 or falls more than 30 mm Hg from baseline.

The Bigger Picture
This isn’t a rare edge case. It’s a systemic failure. Over 22 million Americans take calcium channel blockers. Nearly 8 million get clarithromycin every year. About 1.2 million older adults in the U.S. are prescribed this dangerous combo annually. The Institute for Safe Medication Practices calls it a “high-alert” interaction. That means it’s one of the top 10 most dangerous drug pairs in clinical practice. And yet, awareness is still too low. Only 43% of electronic health record systems have alerts for this interaction. A 2023 study showed that when alerts were added, inappropriate prescribing dropped by 37%. That’s a win. But it shouldn’t take a computer to remind a doctor of a known, life-threatening interaction.What’s Changing Now?
Good things are happening. The STOPP/START criteria - used by doctors across Europe and North America - now explicitly say: “Avoid clarithromycin in patients taking dihydropyridine calcium channel blockers. Use azithromycin instead.” Pharmacogenomics is also stepping in. Some people have a genetic variant (CYP3A5*3/*3) that makes them produce almost no CYP3A5 enzyme. These patients rely almost entirely on CYP3A4. When you give them clarithromycin, their bodies can’t process CCBs at all. A 2021 study found they had more than double the risk of severe hypotension. The message is clear: this interaction is preventable, predictable, and deadly. Yet it keeps happening - because we assume patients will tell us about their meds, or we assume the system will catch it, or we assume it’s “just a little bit” of clarithromycin. It’s not. Even a 5-day course can be enough to cause irreversible damage.Bottom Line
If you’re on a calcium channel blocker - especially nifedipine, amlodipine, or felodipine - clarithromycin is not safe. Azithromycin is. Always ask. Always check. Always insist on the safer alternative. Your blood pressure, your kidneys, and your life depend on it.Can clarithromycin and amlodipine be taken together?
No, they shouldn’t be taken together. While amlodipine carries a slightly lower risk than nifedipine, clarithromycin still increases amlodipine levels by up to 60%, which can cause dangerous drops in blood pressure. Azithromycin is the recommended alternative. Even if you’ve taken both before without issues, the risk is cumulative and can become life-threatening with repeated exposure.
How quickly does the interaction happen?
Symptoms can appear within 24 to 72 hours of starting clarithromycin. The most dangerous drops in blood pressure often occur between days 2 and 4. That’s why monitoring is critical - waiting for symptoms to appear is too late. If you’re on a CCB and start clarithromycin, check your blood pressure daily, especially if you feel dizzy, faint, or unusually tired.
Is azithromycin always the best replacement?
Yes, for most cases where a macrolide is needed. Azithromycin doesn’t inhibit CYP3A4 and has been proven safe with calcium channel blockers in large studies. Other alternatives like doxycycline or amoxicillin may work depending on the infection. But if you need a macrolide - for pneumonia, bronchitis, or chlamydia - azithromycin is the clear, evidence-based choice.
Does this interaction affect people under 65?
Yes. While older adults are at higher risk due to slower metabolism and more chronic conditions, younger people with kidney impairment, heart failure, or on multiple medications can also experience severe hypotension. Age isn’t the only factor - the combination itself is the danger. Anyone on a CCB should avoid clarithromycin regardless of age.
What should I do if I’ve already taken clarithromycin with my blood pressure pill?
Stop taking clarithromycin immediately and contact your doctor. Monitor your blood pressure every few hours. If your systolic pressure drops below 90, you feel lightheaded, confused, or have reduced urine output, go to the emergency room. Acute kidney injury can develop quickly. Don’t wait for symptoms to worsen. The interaction is serious, but catching it early can prevent hospitalization.
Why don’t pharmacies always warn me about this?
Many pharmacy systems still don’t have robust alerts for this interaction, even though it’s been known since at least 2011. Some systems only flag the most extreme cases, or they miss it if the drugs are prescribed by different doctors. Don’t rely on the pharmacy to catch it. Always review your own medications and ask your doctor or pharmacist directly: “Could this antibiotic interact with my blood pressure pills?”
Glendon Cone
December 30, 2025 AT 13:18Bro, I had no idea this was a thing. My grandpa was on amlodipine and got clarithromycin for a cough last year - he nearly passed out in the kitchen. We thought it was just old age. 😳 Now I check every med combo like a hawk. Thanks for the wake-up call.
Henry Ward
December 31, 2025 AT 07:03Of course it’s dangerous - you’re letting Big Pharma push cheaper drugs while people die. This isn’t ‘accidental’ - it’s negligence dressed up as ‘clinical discretion.’ Wake up, people. Your doctor doesn’t care until you’re in the ICU.
Aayush Khandelwal
December 31, 2025 AT 12:10Let’s not sugarcoat this - CYP3A4 inhibition by macrolides is a pharmacokinetic grenade. Clarithromycin’s Ki for CYP3A4 is ~0.1 µM, while azithromycin? Barely registers. It’s not even close. The 5.3x OR in that JAMA paper? That’s not a fluke - it’s a statistical sledgehammer. If your EHR doesn’t flag this, it’s broken.
Sandeep Mishra
December 31, 2025 AT 14:36I’ve seen this happen too. My uncle, 71, on nifedipine for 15 years - got clarithromycin for bronchitis. Ended up in dialysis for a week. I told him to ask about azithromycin next time. He said, ‘But my doctor didn’t say anything.’
That’s the problem. We’ve trained patients to trust, not question. We need to flip that script. Ask. Always ask. It’s not being difficult - it’s being alive.
Joseph Corry
January 1, 2026 AT 08:26How quaint. Another ‘awareness campaign’ about a known interaction from 2011. The real issue isn’t the drug combo - it’s the pathetic state of clinical decision-making in primary care. If your doctor can’t memorize a Class I contraindication, maybe they shouldn’t be prescribing anything at all.
Colin L
January 2, 2026 AT 23:40Let me tell you, I’ve been on both for years - clarithromycin and amlodipine - and nothing happened. So this whole thing is just fearmongering. I’ve got a friend who took it for three weeks straight and he’s fine. Maybe the study is flawed? Maybe it’s just older people with comorbidities? I mean, come on - you’re making it sound like one pill will kill you. It’s not that simple. People have been doing this for decades. Why now? Why the panic? Maybe it’s just media hype. Or maybe the FDA is just trying to push azithromycin because it’s more expensive? I don’t know. I’m just saying - don’t panic. My BP’s fine.
Hayley Ash
January 4, 2026 AT 08:56Wow so if I take a pill for my blood pressure and then another pill for my cough I’m gonna die? What a surprise. Next you’ll tell me water and salt together might cause high BP. Maybe we should just stop taking medicine altogether. Or maybe… just maybe… people should read the damn label. Oh wait they don’t. 🙄
kelly tracy
January 4, 2026 AT 21:17They don’t warn you because they don’t care. They don’t care because they’re making money off your hospital stays. I know this because my mom almost died from this exact combo. The doctor said ‘it’s rare.’ Rare? 1,800 cases in a decade? That’s not rare. That’s a massacre. And now they want you to ‘ask’? No. They should be forced to stop prescribing this. Period.
srishti Jain
January 5, 2026 AT 17:18My aunt did this. Died. Don’t be stupid.
Cheyenne Sims
January 5, 2026 AT 22:35It is imperative to emphasize that the concomitant administration of clarithromycin and dihydropyridine calcium channel blockers constitutes a clinically significant pharmacokinetic interaction, resulting in a marked elevation in plasma concentrations of the latter, thereby precipitating potentially fatal hypotensive episodes. Such a scenario is entirely preventable through appropriate pharmacovigilance and adherence to established clinical guidelines.
Shae Chapman
January 7, 2026 AT 20:13I’m crying. My dad had this happen. He was fine one day, then collapsed at the grocery store. They thought it was a stroke. Turns out it was the combo. He’s okay now but he’s scared to take any meds. 😭 Please, if you’re reading this - ask your doctor. Don’t wait. I’m so glad someone wrote this. Thank you.
Nadia Spira
January 9, 2026 AT 02:05Another ‘educational post’ from someone who probably Googled ‘CYP3A4’ five minutes ago. The real problem isn’t the drug interaction - it’s the fact that we’ve outsourced medical decision-making to algorithms and lazy clinicians. You think an EHR alert fixes this? No. It just makes people click ‘ignore’ and feel better about their negligence. Real change requires systemic overhaul - not a pop-up.
henry mateo
January 10, 2026 AT 00:38wait so azithromycin is safe? i thought it caused heart issues too? i read somethign about QT prolongation… or was that erythromycin? idk i’m confused now. maybe i should just stop taking all pills lol
Kunal Karakoti
January 11, 2026 AT 15:38It’s interesting how we frame this as a ‘dangerous interaction’ when in reality, it’s a symptom of our medical system’s reductionist approach. We treat drugs as isolated entities, not as parts of a living, dynamic system. The body doesn’t recognize ‘drug A’ and ‘drug B’ - it responds to patterns, doses, timing, and individual biochemistry. Maybe the real question isn’t ‘which drug is safer?’ but ‘why are we treating people like chemical equations?’
Kelly Gerrard
January 12, 2026 AT 18:30Every single person reading this needs to immediately contact their prescribing physician and request a medication review. This is not optional. This is not a suggestion. This is a matter of life and death. If your doctor resists, get a second opinion. Your life is worth more than their convenience.