 Feb, 2 2026
Feb, 2 2026
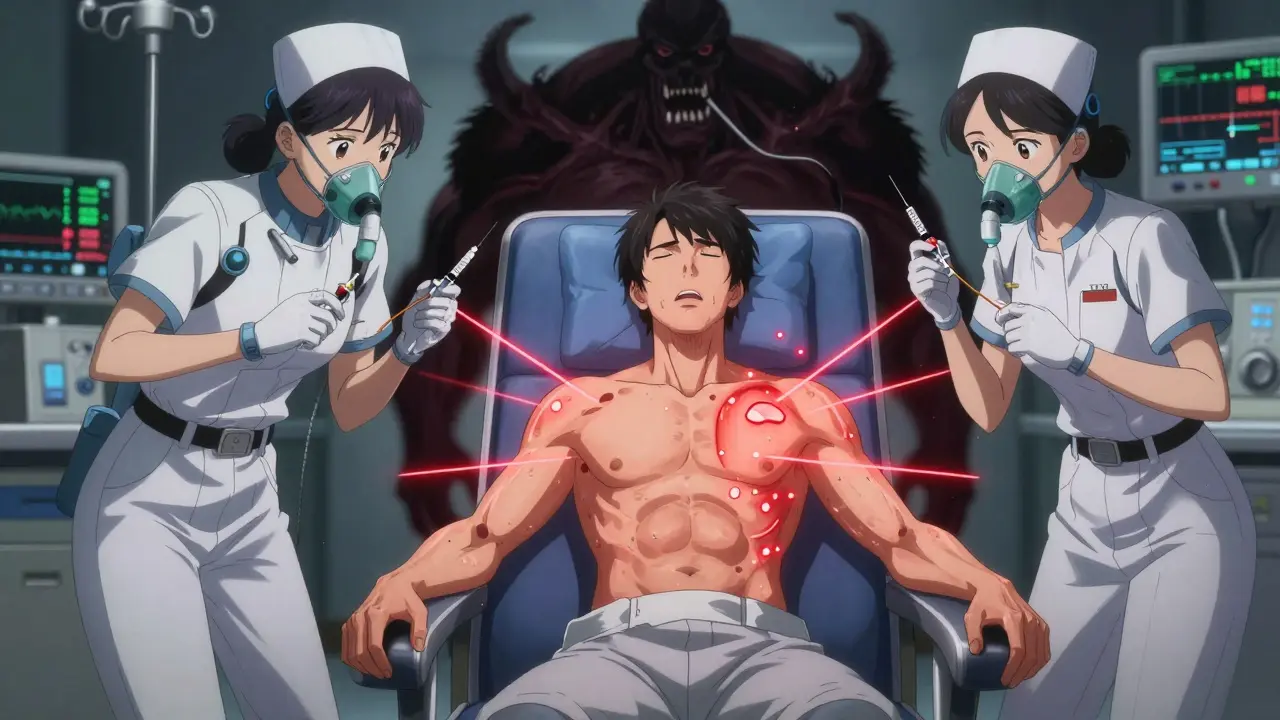
What Happens When Your Body Reacts to Chemo
Chemotherapy saves lives, but for some people, the drugs meant to kill cancer can trigger a dangerous immune response. These are called chemotherapy hypersensitivity reactions. They’re not just nausea or fatigue - they’re real allergic reactions that can turn life-threatening in minutes. About 5% of people getting chemo will have one. Most are mild, but a few can cause breathing failure, low blood pressure, or cardiac arrest. The key isn’t avoiding chemo - it’s knowing the signs and acting fast.
How You’ll Know It’s Happening
Reactions don’t always look the same. Some start with a tickle in your throat. Others begin with a rash or a sudden flush of heat across your chest. Here’s what to watch for, broken down by how your body responds.
- Head and neck: Itchy eyes, runny nose, swelling around your lips or tongue, or a strange metallic taste in your mouth. These might seem small, but they’re early warnings.
- Respiratory: Shortness of breath, wheezing, chest tightness, or coughing that comes out of nowhere. If you’re not sick with a cold and suddenly can’t catch your breath, don’t ignore it.
- Heart and circulation: Dizziness, fainting, rapid heartbeat, or a sudden drop in blood pressure. You might feel like the room is spinning or your vision is tunneling. This isn’t just being tired - it’s your body going into shock.
- Stomach and gut: Nausea, vomiting, cramps, or diarrhea. These are common with chemo, but if they hit hard and fast during an infusion, they’re part of the reaction.
- Skin: Hives, redness, itching, or flushing. About 72% of people report itching. That’s not just dry skin - it’s histamine flooding your system.
- Mind and nerves: A sudden sense of dread, anxiety, or feeling like something terrible is about to happen. Nearly half of people in severe reactions describe this. It’s your body screaming for help before your brain catches up.
Some reactions start mild and explode within minutes. Others creep in hours later. That’s why you need to stay alert even after the IV is done.
Which Chemo Drugs Are Most Likely to Cause This?
Not all chemo drugs are equal when it comes to allergic reactions. Some are far more likely to trigger them - especially if you’ve had them before.
- Platinum drugs: Carboplatin is the biggest culprit. After your sixth treatment, the risk jumps from under 1% to nearly 7%. By the eighth or ninth cycle, it’s over 25%. Cisplatin and oxaliplatin also carry risks, especially with repeated use.
- Taxanes: Paclitaxel and docetaxel are common causes. Up to 30% of people get some kind of reaction, though severe cases are rare.
- Monoclonal antibodies: Drugs like cetuximab, rituximab, and trastuzumab can cause reactions even on the first infusion. These are different from traditional chemo - they’re designed to target cancer cells, but your immune system sees them as invaders.
- Others: L-asparaginase, bleomycin, procarbazine, and cytarabine also show up on the high-risk list.
The more times you get treated, the higher your risk - especially with platinum drugs. That’s why nurses watch you extra closely after cycle five or six.
When It’s an Emergency - The Anaphylaxis Checklist
Anaphylaxis isn’t just a bad reaction. It’s a full-body shutdown. If you have two or more of these, it’s an emergency:
- Low blood pressure (systolic under 90)
- Wheezing or trouble breathing
- Swelling of the tongue or throat
- Rapid heartbeat or fainting
- Sudden skin rash with dizziness
Don’t wait for all of them. If you feel like you’re dying - even if you’re not sure why - tell your nurse immediately. Anaphylaxis doesn’t get better with antihistamines alone. It needs epinephrine. Fast.
What the Team Does When a Reaction Happens
Every chemo unit should have a plan. Here’s what happens when a reaction hits.
- Stop the infusion. No exceptions. Even if it’s just a little itching, they stop the drug.
- Call for help. Nurses alert the team. Anaphylaxis kits are pulled - epinephrine, oxygen, IV fluids.
- Give epinephrine. If it’s severe, they inject 0.3-0.5 mg into your thigh. This is the only thing that can reverse airway swelling and low blood pressure. It works in seconds.
- Support your body. Oxygen through a mask, IV fluids to raise blood pressure, antihistamines like diphenhydramine, and steroids like dexamethasone to calm the immune response.
- Monitor you closely. Your heart rate, blood pressure, and oxygen levels are tracked nonstop for at least an hour after symptoms fade.
For mild reactions, they might slow the drip and restart after 30 minutes. For severe ones, the chemo is stopped for good - unless you go through a special desensitization process.

How They Try to Prevent Reactions Before They Start
Prevention isn’t luck. It’s a routine.
For drugs like paclitaxel or docetaxel, you’ll get premeds before the infusion:
- Dexamethasone (20 mg IV) - 12 and 6 hours before
- Diphenhydramine (50 mg IV) - 30 minutes before
- Famotidine (20 mg IV) - 30 minutes before
This combo reduces the chance of a reaction by up to 70%. Slower infusion rates also help. Instead of dumping the drug in 15 minutes, they stretch it over an hour or more.
If you’ve had a reaction before, your team will avoid that drug unless there’s no other option. Then, they’ll use desensitization - slowly giving you tiny amounts of the drug over 4 to 12 hours while watching you like a hawk. It’s risky, but it lets people keep using a drug that works.
What You Need to Do - Even After Treatment Ends
You’re not safe just because the IV is out.
Some reactions show up hours later. You might feel fine leaving the clinic, then get a rash or chest tightness at home. That’s why every patient gets the same warning: Call your nurse if you feel anything unusual - even if it’s not what you’ve felt before.
Keep a list of every chemo drug you’ve had and any reaction you had. Bring it to every appointment. Tell every new doctor, nurse, or pharmacist. Write it in your phone. Don’t assume they’ll know.
And if you’ve had a severe reaction, make sure your family knows the signs. If you collapse at home, they need to know to call 999 and use your epinephrine auto-injector if you have one.
Why This Matters More Than You Think
Chemotherapy hypersensitivity isn’t rare. It’s predictable. And it’s preventable - if you know the signs and speak up.
Too many people dismiss early symptoms as "just side effects." But itching, flushing, or dizziness during chemo aren’t normal fatigue. They’re your body’s alarm system. Nurses are trained to catch them. But they can’t read your mind.
If you feel off - even a little - say something. If you’ve had a reaction before, remind them. If you’re scared, say that too. Your voice could save your life.
Can chemotherapy hypersensitivity happen on the first treatment?
Yes. While some reactions build up over time - especially with platinum drugs - others like monoclonal antibodies (cetuximab, rituximab) can trigger a reaction on the very first infusion. That’s why all patients are closely monitored during the first dose, even if they’ve never had an allergy before.
Is a chemo reaction the same as a chemo infusion reaction?
Not always. Infusion reactions can be caused by the drug itself irritating your body - not your immune system. These might cause fever, chills, or muscle aches. Hypersensitivity reactions are true allergic responses, triggered by your immune system releasing histamine and other chemicals. The symptoms overlap, but the treatment differs. Anaphylaxis requires epinephrine; a simple infusion reaction might just need a slower drip.
How do they test for a chemo allergy?
There’s no simple skin test like for peanuts. Doctors use a mix of clinical history and lab tests. Blood tests can check for elevated tryptase (a marker of mast cell activation) or specific IgE antibodies to the drug. Basophil activation tests, which measure how your immune cells react to the drug in a lab, are also used in specialized centers. But often, the diagnosis comes from what happened during the infusion - symptoms plus timing.
If I had a reaction, will I ever get that chemo again?
Usually, they avoid the drug that caused the reaction. But if it’s the best option for your cancer, you might go through a desensitization protocol. This means getting tiny, increasing doses over several hours under close watch. It’s not risk-free, but it lets people keep using life-saving drugs they’re allergic to. This is only done in hospitals with the right equipment and staff.
What should I carry with me after having a chemo reaction?
Always carry a list of the chemo drugs you’ve had and which ones caused reactions. If you’ve had a severe reaction, ask your oncologist if you should carry an epinephrine auto-injector (like an EpiPen) and a medical alert bracelet. Make sure your family knows where it is and how to use it. Don’t assume emergency responders will know your history unless you tell them.
Can I prevent chemo reactions with over-the-counter antihistamines?
No. Taking Benadryl on your own before chemo won’t help - and might mask early warning signs. Only use medications given by your oncology team. Premedication is carefully timed and dosed based on the drug you’re getting. Self-medicating could delay recognition of a serious reaction and put you at greater risk.
Wendy Lamb
February 3, 2026 AT 10:48Just had my 7th cycle of carboplatin last week. Started with a weird metallic taste and itchy palms-ignored it thinking it was just "chemo vibes." Thank god the nurse noticed the flush and stopped it. They gave me epinephrine and I was fine. Don’t brush off the small stuff. Your body knows before your brain does.