 Feb, 1 2026
Feb, 1 2026
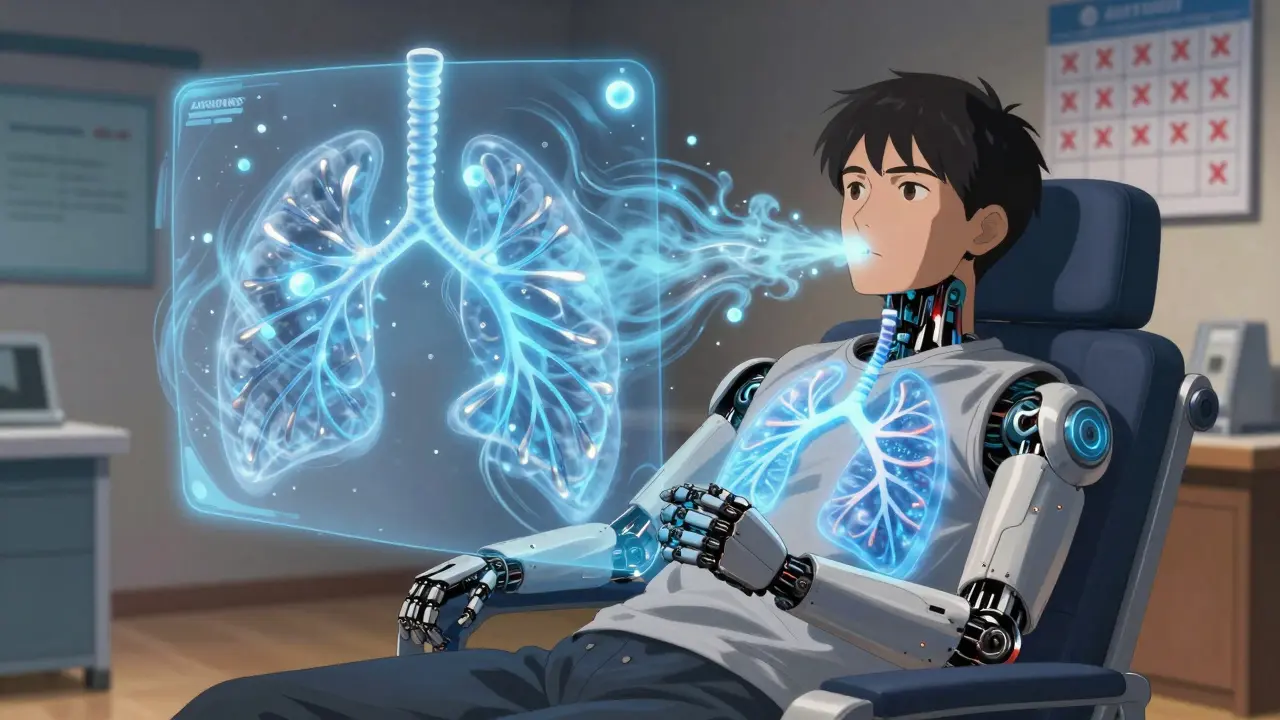
What Bronchiectasis Really Feels Like
You wake up with a cough that won’t quit. Not the kind that fades after a cold, but a deep, wet rattle that’s been there for months-maybe years. You’re spitting out thick, yellow-green mucus every morning, sometimes more than a coffee cup’s worth. It smells bad. You’re tired. Your chest feels heavy, even when you’re not sick. This isn’t just a bad habit or allergies. This is bronchiectasis.
Bronchiectasis isn’t a one-time infection. It’s permanent damage to your airways. The tubes that carry air in and out of your lungs have stretched and weakened over time, losing their ability to clear mucus. That mucus sits there, breeding bacteria. Infection follows. Inflammation follows. More damage follows. It’s a cycle, and once it starts, it doesn’t stop unless you actively break it.
The Three Pillars of Control
There’s no cure. But you can live well with it-if you treat it right. Experts agree: three things matter most. Airway clearance. Antibiotics. And consistency.
Forget the idea that coughing hard will help. That’s not how it works. Bronchiectasis needs smart, scheduled techniques to move mucus out before it turns into a breeding ground. Think of it like cleaning a clogged drain. You don’t just pour bleach in once a year. You flush it daily.
Clearing Your Airways: It’s Not Optional
Doctors don’t just recommend airway clearance. They demand it. The American Thoracic Society calls it Grade A-strongest possible recommendation. Why? Because the numbers don’t lie.
Patients who do daily clearance have 47% fewer hospital visits. Their lung function declines by 28 mL per year. Those who skip it? 45 mL. That’s not a small difference. That’s losing your breath faster.
There are tools. The high-tech option is a vibrating vest-costs $5,000 to $7,000. But most people don’t need it. Handheld PEP devices like the Aerobika® cost under $200. They work just as well for most. You breathe in, hold, then exhale slowly through the device. The resistance pushes mucus up. Then you huff.
Huff coughing isn’t a regular cough. It’s a controlled burst-three types: low, medium, high lung volume. You don’t gag. You don’t strain. You exhale like you’re fogging a mirror. Do it right, and mucus comes out in chunks. Do it wrong? Nothing moves. Most people need 12 sessions with a respiratory therapist to get it right. Don’t skip this step.
Do it twice a day. Fifteen to twenty minutes each time. If you’re busy, do it while watching TV. If you’re tired, do it in the morning before coffee. But do it. Every day.
Antibiotics: The Right Way, Not the Easy Way
When you get sick, you grab antibiotics. That’s natural. But with bronchiectasis, that’s how resistance starts.
Studies show 38% of patients develop antibiotic-resistant bugs within five years of using them only during flare-ups. That’s not a risk. That’s a trap.
The better path? Prophylaxis. Low-dose, regular antibiotics. Azithromycin-250 to 500 mg, three times a week-is the gold standard. Not daily. Not just when you feel bad. Three times a week, year-round. The EMBRACE trial showed this cuts flare-ups by 32%. That’s not magic. That’s science.
For people with Pseudomonas-a stubborn bug that loves damaged lungs-inhaled antibiotics like tobramycin can cut colonization by 56%. These aren’t pills. They’re nebulized. You breathe them in. They hit the lungs directly. Less side effects. More power.
And here’s the catch: antibiotics alone don’t work. If you’re taking them but skipping airway clearance, you’re just feeding resistant bacteria. The European Respiratory Society says patients who only use antibiotics during flare-ups are 2.3 times more likely to lose lung function permanently.
What Helps Beyond the Basics
Some things make daily life easier. Hypertonic saline-7% salt water-nebulized daily thins mucus. It’s not a cure, but it makes huffing work better. Most patients say it’s the difference between struggling and getting air out.
Dornase alfa, a drug used in cystic fibrosis, also helps break down thick mucus. It’s expensive, but if your mucus is like glue, it’s worth asking about.
Bronchodilators? They help a little-but only if you use them with clearance. Alone, they improve symptoms by 12%. With clearance? 28%. Combine them. Don’t skip the combo.
Hydration matters. Drink at least two liters of water a day. Thinner mucus moves easier. Simple. But forgotten.
The Real Hurdles: Time, Cost, and Burnout
Let’s be honest. Doing this every day is exhausting.
Forty-two percent of people on NHS forums say they can’t keep up because of work, kids, or just plain fatigue. You’re not lazy. You’re human.
Insurance won’t always cover the Aerobika®. Some patients pay out of pocket. Others borrow devices from clinics. Ask your respiratory therapist. Many hospitals have loaner programs.
And the education? It’s uneven. Only 40% of clinics give you illustrated guides in your language. If you’re not getting clear instructions, ask for a video or a printed handout. Don’t settle.
There are apps now. The American Thoracic Society’s “Clearing the Air” app lets you track your daily clearance, symptoms, and antibiotic days. It’s free. Use it. Accountability helps.
What’s New? What’s Coming?
There’s hope on the horizon. In 2023, the FDA approved gallium maltolate, an inhaled treatment for stubborn Pseudomonas infections. Early results show 42% fewer flare-ups.
Researchers are testing inhaled bacteriophages-viruses that target bacteria. In early trials, they cleared resistant infections in 68% of cases. It’s experimental, but it’s real.
Genetic testing is starting to identify who’s at risk for rapid decline. By 2025, treatment may be personalized-not just based on symptoms, but on your DNA.
But none of this replaces daily clearance. Not yet. Not ever, probably. The foundation hasn’t changed.
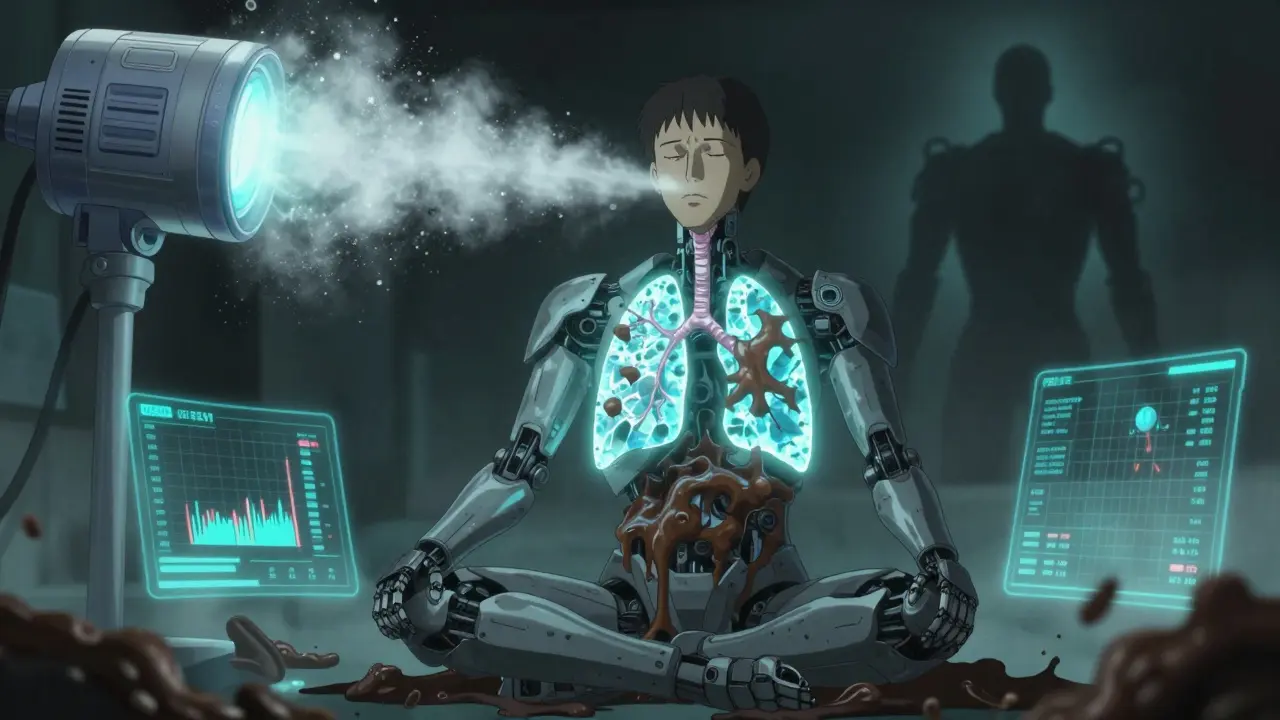
What Happens If You Don’t Do Anything?
Progression is slow. But it’s steady.
Without treatment, FEV1 drops 30-50 mL per year. That’s like losing 10% of your lung capacity every five years. You’ll need oxygen. You’ll get hospitalized more. You might need surgery to remove a damaged lobe.
One in five people with bronchiectasis eventually needs oxygen. Five percent need surgery. These aren’t rare outcomes. They’re predictable ones.
And here’s the worst part: the damage is permanent. You can’t undo it. But you can stop it from getting worse.
Your Action Plan
- Get a chest CT scan if you haven’t already. It’s the only way to confirm bronchiectasis.
- See a respiratory therapist. Learn huff coughing and PEP device use. Don’t guess.
- Start daily airway clearance. Two sessions. 15-20 minutes each. Set a phone reminder.
- Ask your doctor about azithromycin 250-500 mg three times a week. Don’t wait for a flare-up.
- Nebulize 7% hypertonic saline daily. It’s cheap. It helps.
- Drink two liters of water a day. No exceptions.
- Track your symptoms. Use the “Clearing the Air” app or a notebook.
- Join a support group. The Bronchiectasis and NTM Initiative has monthly virtual meetings. You’re not alone.
Final Thought
Bronchiectasis doesn’t kill quickly. It steals slowly. Your breath. Your energy. Your freedom.
But you’re not powerless. Every day you clear your airways, you’re pushing back. Every time you take your antibiotic, you’re breaking the cycle. Every sip of water, every huff, every session with your therapist-it adds up.
This isn’t about being perfect. It’s about being consistent. Even on the days you’re tired. Even when it feels pointless.
Because the alternative? It’s worse.
Can bronchiectasis be cured?
No, bronchiectasis cannot be cured. The damage to the airways is permanent. But with consistent treatment-daily airway clearance, targeted antibiotics, and proper hydration-the progression of the disease can be slowed dramatically. Many people live full, active lives for decades with proper management.
How long does it take to see results from airway clearance?
Most people notice less coughing and easier breathing within 2-4 weeks of starting daily clearance. But it takes 6-8 weeks to build the habit and master the technique. The real benefit-fewer hospital visits and slower lung decline-shows up over months and years. This is a long-term game.
Is it safe to take antibiotics long-term for bronchiectasis?
Yes, when used correctly. Low-dose, non-daily antibiotics like azithromycin (250-500 mg three times a week) are safe for years. They reduce inflammation and prevent infections without causing the same side effects as daily use. The key is combining them with airway clearance. Using antibiotics only during flare-ups increases the risk of resistant bacteria.
Do I need a special device for airway clearance?
Not necessarily. You can do effective clearance with just breathing techniques like the Active Cycle of Breathing Techniques (ACBT) and huff coughing. But handheld PEP devices like the Aerobika® make it easier and more consistent. They cost under $200 and are often covered by insurance. Vests are powerful but expensive and usually only needed for severe cases.
What if I can’t afford treatment or devices?
Many hospitals and clinics have loaner programs for PEP devices. Ask your respiratory therapist. Hypertonic saline and hydration cost very little. The most important tool-your breathing and huff coughing-costs nothing. Focus on mastering those first. Community support groups and apps like “Clearing the Air” are free. You don’t need expensive gear to start controlling your symptoms.
Can bronchiectasis get worse even if I follow treatment?
Yes, but much more slowly. Some people have genetic factors or other conditions that make progression faster. But adherence to daily clearance and antibiotics still reduces hospitalizations by nearly half and cuts lung function decline by almost 40%. It’s not a guarantee, but it’s the best defense we have.
How do I know if I have bronchiectasis and not just chronic bronchitis?
Chronic bronchitis means you’ve had a cough with mucus for at least three months a year for two years, usually from smoking. Bronchiectasis is structural damage confirmed by a CT scan. You’ll see dilated airways-wider than the blood vessels next to them. Bronchiectasis also causes foul-smelling sputum, frequent infections, and sometimes coughing up blood. A CT scan is the only way to be sure.
Is it okay to stop antibiotics if I feel better?
No. If you’re on prophylactic antibiotics like azithromycin, stopping them-even when you feel fine-lets bacteria rebuild in your airways. You’ll likely have another flare-up within weeks. Prophylaxis works because it’s continuous. It’s not about how you feel. It’s about preventing infection before it starts.
Dan Pearson
February 2, 2026 AT 06:20larry keenan
February 2, 2026 AT 16:59