 Dec, 1 2025
Dec, 1 2025
More than 40% of adults in the U.S. take at least one medication that can react dangerously with alcohol. Yet most people don’t realize how risky it can be to have even one drink while on pills. It’s not just about getting drunk faster-it’s about your liver shutting down, your breathing slowing to a stop, or your stomach bleeding internally. These aren’t rare accidents. They happen every day, often because no one ever told the patient what to watch for.
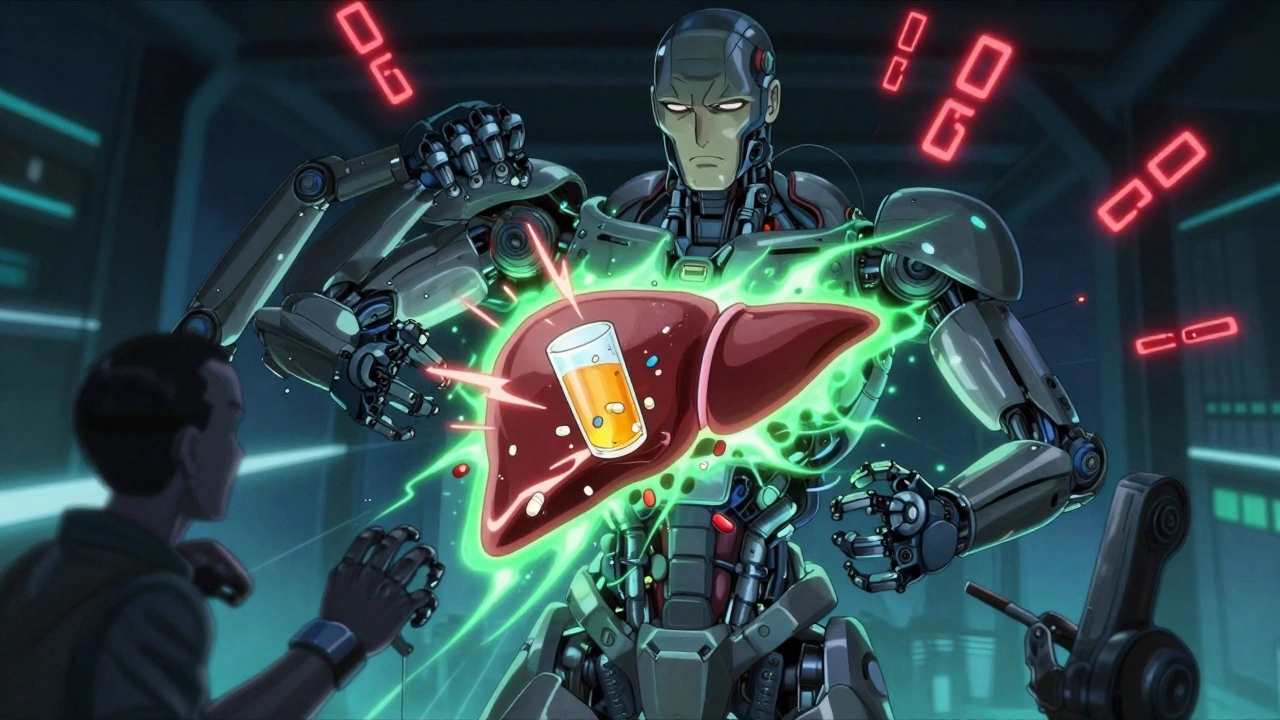
How Alcohol and Medicines Fight Inside Your Body
Your liver is the main battlefield. It uses enzymes-especially CYP2E1, CYP3A4, and CYP1A2-to break down both alcohol and most medications. When you drink while taking medicine, they fight for the same tools. This causes two major problems.
First, alcohol can slow down how fast your body clears the medicine. That means the drug builds up in your system. A dose that’s normally safe can become toxic. For example, mixing alcohol with diazepam (Valium) can stretch its half-life from 20-100 hours to 35-150 hours. That’s like taking five doses in one day without realizing it.
Second, alcohol can make the medicine’s effects stronger. This is especially true for drugs that calm your nervous system-like sleep aids, anti-anxiety pills, or painkillers. When alcohol joins them, it’s like adding gasoline to fire. Together, they can depress your breathing so much that you stop breathing altogether. Studies show this combo increases GABA activity in the brain by 400%, even at low alcohol levels like 0.05%-just half the legal driving limit.
Medications That Are Especially Dangerous with Alcohol
Not all drugs react the same way. Some are silent killers when mixed with alcohol. Here are the top offenders:
- Metronidazole (Flagyl) - One drink can trigger a violent reaction: flushing, vomiting, racing heart, chest pain. In 92% of cases, symptoms hit within minutes. This isn’t a side effect-it’s a chemical explosion caused by blocked alcohol breakdown.
- Benzodiazepines (Xanax, Valium, Ativan) - These are the #1 cause of alcohol-medication deaths. The combination causes extreme drowsiness, confusion, and respiratory failure. CDC data shows they account for 32% of all fatal interactions.
- Opioids (Oxycodone, Morphine, Hydrocodone) - Alcohol makes these drugs 8 times more likely to stop your breathing. The CDC calls this one of the deadliest combinations in modern medicine.
- Antidepressants (SSRIs like Prozac, Zoloft) - Alcohol doesn’t just make you feel more drunk-it makes the depression worse. Studies show it extends the time you feel intoxicated by over 3 hours. It also raises the risk of dizziness, fainting, and liver damage.
- Acetaminophen (Tylenol) - Even a few drinks a day while taking regular doses of Tylenol can trigger sudden liver failure. A 2023 study found 18% of patients had elevated liver enzymes after just moderate alcohol use with standard Tylenol doses.
- NSAIDs (Ibuprofen, Naproxen) - Mixing these with alcohol increases stomach bleeding risk by 300-500%. You might not feel pain until it’s too late.
- Antihistamines (Benadryl) - These are in cold and allergy meds. With alcohol, they turn into sedatives. People report falling asleep while driving or not waking up after a nap.
The Hidden Risks in Over-the-Counter Pills
Many people think only prescription drugs are dangerous with alcohol. That’s a myth. You’re more likely to get hurt from something you bought without a prescription.
Take Benadryl. It’s in sleep aids, cold medicines, and allergy pills. One pill with a glass of wine can make you so sleepy you can’t stand up. The FDA’s own database shows its sedative effect triples with alcohol.
Or consider NyQuil. It contains acetaminophen, dextromethorphan, and doxylamine-all of which react badly with alcohol. People think it’s “just a cold medicine,” but it’s essentially a cocktail of depressants. Emergency rooms see dozens of cases every month from people who drank while taking it.
Even aspirin or ibuprofen can cause internal bleeding if you drink regularly. You might not notice until you’re vomiting blood or passing black stools. No warning label says “don’t drink.” But the science is clear.
Who’s Most at Risk-and Why
Age matters. After 65, your liver processes alcohol 35% slower. That means even small amounts stick around longer, increasing interaction risk. The American Geriatrics Society lists 17 medications that are especially dangerous for older adults.
Women are more vulnerable too. On average, they have less body water and more fat, so alcohol concentrates faster in their blood. A woman who drinks two drinks may have the same blood alcohol level as a man who drinks three.
And then there’s polypharmacy. Nearly half of all U.S. adults take at least one prescription drug. Two in three seniors take five or more. Each new pill adds another chance for alcohol to interfere. The FDA now calls alcohol-medication interactions the third most common cause of serious drug reactions.
What You Should Do-Step by Step
You don’t have to quit alcohol forever. But you do need to be smart. Here’s what works:
- Check every new prescription - Ask your doctor or pharmacist: “Is it safe to drink alcohol with this?” Don’t assume they’ll tell you. Only 42% of prescription bottles include alcohol warnings.
- Use a trusted tool - WebMD and GoodRx have interaction checkers. But only 37% of online tools are accurate. Stick to ones that cite FDA or NIAAA guidelines.
- Know your standard drinks - One drink = 12 oz beer, 5 oz wine, or 1.5 oz spirits. Anything more counts as multiple drinks.
- Wait 72 hours before starting high-risk meds - For metronidazole, tinidazole, or disulfiram, stop drinking at least three days before your first dose. This cuts reaction risk from 92% to 8%.
- If you drink, do it safely - Wait 2-3 hours after taking your pill. Eat food first. Limit yourself to one drink for women, two for men. Never drink on an empty stomach.
- Watch for warning signs - Flushing, nausea, rapid heartbeat, dizziness, confusion, trouble breathing. If you feel any of these, stop drinking and call your doctor.

Why Most People Don’t Get the Right Advice
Doctors rarely bring it up. A 2022 AARP survey found 68% of patients were never warned about alcohol interactions. Pharmacists are better-but only if you ask.
Walgreens found that 89% of patients changed their drinking habits after a pharmacist gave them a simple warning. But only 1 in 4 people ever ask.
Even the labels are unreliable. A 2022 study showed patients understood only 48% of the written warnings on their meds. Visual charts-like the ones from Injury Matters Foundation-boost understanding to 82%. Ask your pharmacist if they have one.
What’s Changing-And What’s Coming
Things are slowly getting better. Starting January 2024, the FDA requires new prescription labels to include pictograms showing alcohol risks. That means a simple icon-like a glass with a red slash-on high-risk drugs.
Telehealth platforms now screen for alcohol use during virtual visits. Medicare Part D plans must flag risky combinations by December 2024. And Stanford’s AI system reduced dangerous mixes by 37% in just six months.
But the biggest gap remains education. Only 39% of medical schools teach alcohol-medication interactions as a standalone topic. That means many doctors still don’t know the full picture.
Real Stories, Real Consequences
One man took metronidazole for a tooth infection. He had one beer at dinner. Within 20 minutes, he was in the ER with a heart rate of 180 and vomiting. He didn’t know the drug and alcohol combo could do that.
A woman took Xanax for anxiety and drank wine to relax. She fell asleep in her car and woke up hours later with no memory of how she got home. She didn’t realize the combination could make her pass out.
Another patient took Tylenol for a headache after a few glasses of wine. Three days later, his liver failed. He didn’t know “moderate drinking” could be deadly with acetaminophen.
These aren’t outliers. They’re common. And they’re preventable.
Can I have one drink with my medication?
It depends on the medication. For some, like metronidazole or benzodiazepines, even one drink can be dangerous. For others, like SSRIs or NSAIDs, one drink may be okay if you’re healthy and don’t drink often. Always check with your doctor or pharmacist. Never assume it’s safe.
How long should I wait after taking medicine before drinking alcohol?
For most medications, wait at least 2-3 hours after your dose. But for long-acting drugs like diazepam or antidepressants, the drug stays in your system for days. In those cases, avoid alcohol entirely. For metronidazole, stop drinking at least 72 hours before your first dose and wait 72 hours after your last dose.
Is it safe to drink alcohol while taking Tylenol?
It’s risky. Taking more than 3 alcoholic drinks a day with Tylenol can cause serious liver damage. Even one or two drinks daily with regular Tylenol doses can raise liver enzyme levels, a sign of early damage. If you drink regularly, avoid Tylenol. Use ibuprofen instead-but only if you don’t have stomach issues.
Do all doctors know about alcohol-medication risks?
No. Only 39% of medical schools teach this topic in depth. Many doctors assume patients know-or they forget to mention it. That’s why you need to ask. Don’t wait for them to bring it up.
Can I drink alcohol if I’m taking antibiotics?
Most antibiotics are fine with alcohol-except for metronidazole, tinidazole, and linezolid. These cause severe reactions. Azithromycin and amoxicillin are generally safe. But alcohol can weaken your immune system, making it harder to recover. If you’re sick, it’s best to skip alcohol until you’re fully healed.
What should I do if I accidentally mixed alcohol with my medication?
Stop drinking immediately. Watch for symptoms: dizziness, nausea, rapid heartbeat, trouble breathing, confusion, or fainting. If you have any of these, call 911 or go to the ER. Even if you feel fine, call your doctor. Some reactions happen hours later.
If you’re taking multiple medications, keep a list-both prescription and over-the-counter-and bring it to every appointment. Ask your pharmacist to review it for alcohol risks. It’s a five-minute conversation that could save your life.
patrick sui
December 3, 2025 AT 04:23Whoa. This is wild. CYP2E1 and CYP3A4 are the real MVPs (or villains?) here. I had no idea alcohol could stretch diazepam’s half-life that much. It’s like your liver is juggling chainsaws while blindfolded. 🤯
Conor Forde
December 4, 2025 AT 18:51Y’all are acting like this is news. My grandad died from mixing Tylenol and whiskey. He thought ‘moderate’ meant ‘a couple shots after his pills.’ Guess what? It didn’t. RIP. 🍷💀
Declan O Reilly
December 6, 2025 AT 09:03Think about it - we treat alcohol like a chill buddy, but it’s actually the sneaky saboteur in your biochemistry. It doesn’t just ‘add’ to meds, it hijacks your metabolic pathways like a hacker in a Netflix thriller. We need to reframe this. It’s not ‘don’t drink with meds’ - it’s ‘don’t invite chaos into your cells.’ 🌱
Adrian Barnes
December 7, 2025 AT 07:40It is both alarming and unsurprising that 68% of patients receive no warning. This represents a systemic failure in patient education, compounded by physician complacency and regulatory inertia. The CDC data cited is statistically significant, yet the dissemination of this information remains fragmented and anecdotal. One must question the ethical obligations of prescribers in light of this evidence.
Declan Flynn Fitness
December 9, 2025 AT 00:20Bro, I’ve seen so many people down Benadryl with wine like it’s a nightcap. One time my buddy passed out on the couch after a glass and a pill. Scared the hell out of us. 😅 Just say no to sleepy cocktails. Your liver will thank you. #StaySafe
Jaswinder Singh
December 9, 2025 AT 11:02You people act like this is some deep secret. My cousin died at 42 from liver failure after drinking while on Tylenol. He didn’t even know it was dangerous. Stop pretending this is ‘just advice.’ This is a death sentence waiting to happen. And yeah, I’m angry. Because nobody told him.
Bee Floyd
December 11, 2025 AT 10:11Love how you broke this down. The FDA’s new pictogram rule? Long overdue. I’ve seen so many patients skip the tiny text on labels. A simple 🚫🍷 icon might actually save lives. Also - never assume your pharmacist knows your full med list. Bring a list. Always. 🙏
Jeremy Butler
December 12, 2025 AT 01:30The notion that alcohol interacts with medications on a biochemical level is not merely a clinical observation; it is a manifestation of the inherent antagonism between exogenous psychoactive substances and endogenous homeostatic mechanisms. The liver, as the principal site of xenobiotic metabolism, functions under a principle of competitive inhibition - a concept well-established in pharmacokinetics since the mid-20th century. The failure of public health messaging to reflect this complexity is not an oversight - it is a philosophical deficit in medical education.