 Oct, 14 2025
Oct, 14 2025
Muscle Relaxant Decision Tool
Find Your Best Muscle Relaxant Match
Answer a few quick questions about your condition and health profile to get personalized recommendations.
Your Recommended Muscle Relaxant
Why this matches your profile:
Key considerations:
When a painful muscle spasm keeps you up at night, the instinct is to reach for a drug that promises quick relief. But not every muscle relaxants works the same way, and picking the right one can feel like a guessing game. This guide breaks down Baclofen, how it stacks up against the most common alternatives, and what you should really consider before swallowing that next pill.
What Is Baclofen?
Baclofen is a GABA‑B receptor agonist prescribed to reduce spasticity and painful muscle contractions. First approved in the 1970s for multiple sclerosis‑related spasticity, it’s now a staple for anyone dealing with chronic muscle tightness.
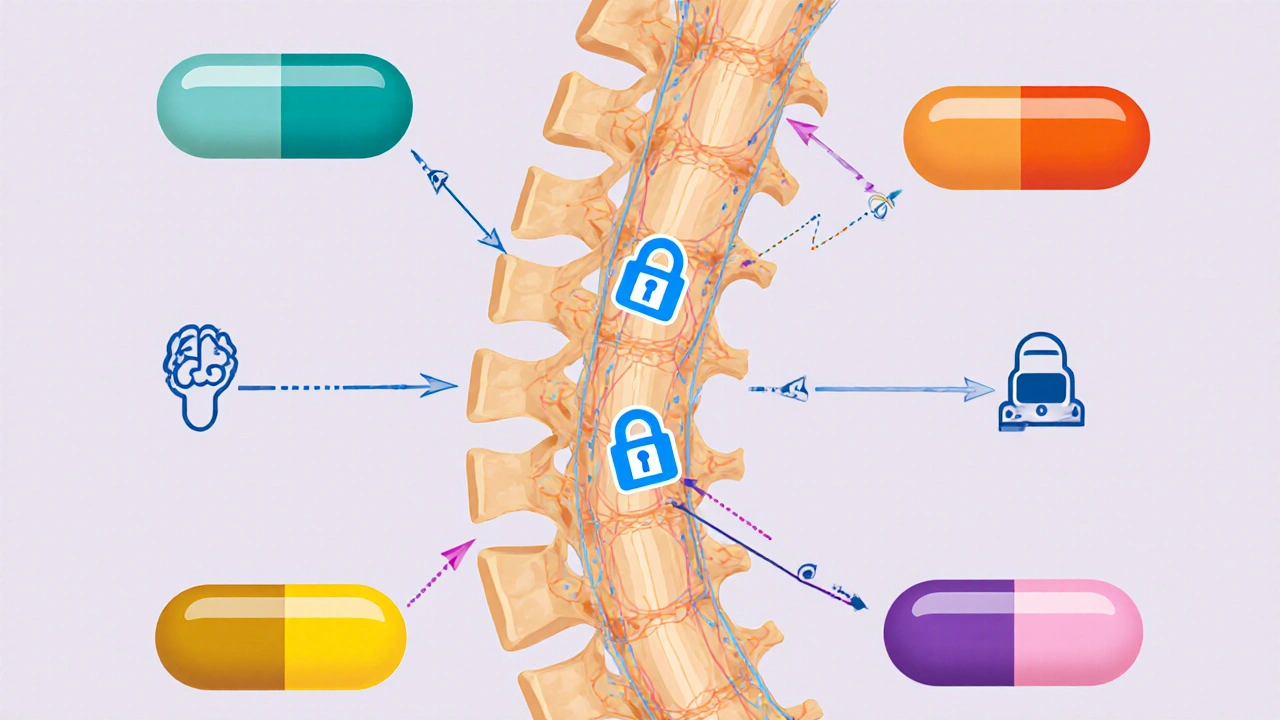
How Baclofen Works
Unlike many over‑the‑counter relaxers that act on the central nervous system more broadly, Baclofen targets the GABA‑B receptors in the spinal cord. By inhibiting the release of excitatory neurotransmitters, it dampens the signal that tells your muscles to contract. The result is a smoother, more controlled stretch of the affected muscle groups. Most patients start with a low dose-usually 5mg three times a day-and titrate up to a maximum of about 80mg per day, depending on tolerance and therapeutic response.
Top Alternatives to Baclofen
When Baclofen isn’t enough, or you experience side‑effects, clinicians often turn to other agents. Below are the five most widely used alternatives, each with its own mechanism and profile.
- Tizanidine is an alpha‑2 adrenergic agonist that reduces muscle tone by decreasing spinal interneuron activity. It works quickly, often within an hour, making it a good rescue option.
- Cyclobenzaprine is a tricyclic‑derived muscle relaxant that acts mainly in the brainstem to interrupt pain signals. It’s commonly prescribed for short‑term acute muscle strains.
- Methocarbamol is a centrally acting carbamate that provides mild sedation while relaxing skeletal muscles. Its onset is slower, but it tends to cause less dizziness than some peers.
- Diazepam is a benzodiazepine that enhances GABA‑A activity, producing both muscle relaxation and anxiolysis. Because of its potential for dependence, it’s usually reserved for severe spasticity or when anxiety worsens the muscle tone.
- Gabapentin is an anticonvulsant that modulates calcium channels, indirectly reducing neuropathic pain and associated muscle spasm. It’s a favorite for patients whose spasticity has a strong nerve‑pain component.
Side‑Effect Profile Comparison
| Medication | Common Side‑Effects | Serious Risks | Typical Starting Dose | Maximum Recommended Dose |
|---|---|---|---|---|
| Baclofen | Drowsiness, weakness, dizziness | Withdrawal seizures if stopped abruptly | 5mg three times daily | 80mg per day |
| Tizanidine | Dry mouth, fatigue, hypotension | Liver toxicity with prolonged high doses | 2mg up to three times daily | 36mg per day |
| Cyclobenzaprine | d>Dry mouth, constipation, sedation | Cardiac arrhythmias (rare) | 5mg three times daily | 30mg per day |
| Methocarbamol | Drowsiness, headache, dizziness | Rare hepatotoxicity | 500mg three times daily | 4000mg per day |
| Diazepam | Blurred vision, ataxia, sedation | Dependence, respiratory depression | 2-5mg two to three times daily | 40mg per day |
| Gabapentin | Peripheral edema, dizziness, fatigue | Suicidal ideation in predisposed patients | 300mg three times daily | 3600mg per day |
The table makes it clear that every option has trade‑offs. Baclofen’s biggest red flag is the risk of severe withdrawal if you tap out too quickly-a problem you don’t see as often with Tizanidine or Gabapentin.

Choosing the Right Muscle Relaxant
Here’s a quick decision framework you can use the next time a doctor asks which drug to try first:
- Is the spasticity chronic or acute? For long‑term, Baclofen and Diazepam are the go‑to choices; for short bursts of pain, Cyclobenzaprine or Methocarbamol may be enough.
- Do you have liver or kidney concerns? Tizanidine and Diazepam need liver monitoring, while Gabapentin is cleared renally.
- Is sedation a deal‑breaker? If you need to stay alert-say, for driving-Methocarbamol and Gabapentin usually cause less drowsiness than Baclofen or Diazepam.
- Are you prone to dependence? Avoid benzodiazepines like Diazepam unless no other option works.
- Cost and insurance coverage? Generic Baclofen and Methocarbamol are often the cheapest; newer agents like Tizanidine may cost more.
Take the list and match it to your personal health profile. In many cases, a combination works best-low‑dose Baclofen for baseline control, plus a short‑acting agent like Tizanidine for flare‑ups.
Practical Tips & Common Pitfalls
- Taper, don’t quit cold turkey. Reduce Baclofen by 5mg every 3-5 days to avoid seizures.
- Watch for drug interactions. Baclofen can amplify the sedative effect of alcohol, antihistamines, or other CNS depressants.
- Monitor blood pressure. Tizanidine can cause a sudden drop; check your BP before each dose if you have a history of hypotension.
- Stay hydrated. Some patients develop constipation with Cyclobenzaprine-drink plenty of fluids and consider a fiber supplement.
- Schedule regular labs. Liver function tests every 3months for Tizanidine, kidney function for Gabapentin.
Remember, medication is just one piece of the puzzle. Physical therapy, stretching routines, and proper ergonomics can boost any drug’s effectiveness.
Frequently Asked Questions
Can I use Baclofen while pregnant?
Animal studies suggest a risk of fetal harm, and human data are limited. Most clinicians classify Baclofen as Category C, meaning you should only take it if the potential benefit outweighs the risk. Discuss alternatives with your obstetrician.
How long does it take for Baclofen to start working?
Oral Baclofen usually begins to reduce spasticity within 2-4hours, reaching its full effect after a few days of consistent dosing.
Is Baclofen addictive?
Physical dependence can develop, especially at higher doses, but true addiction (craving, compulsive use) is rare compared with benzodiazepines.
Can I combine Baclofen with a benzodiazepine?
The combo can boost muscle relaxation but also increase sedation and respiratory depression. It should only be done under close medical supervision.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next one. In that case, skip the missed dose-don’t double‑up.
Sherine Mary
October 14, 2025 AT 17:30Reading through the comparison, several points jump out that are worth emphasizing. First, the distinction between chronic and acute spasticity is not merely academic; it dictates the pharmacodynamics of each agent. Baclofen, as a GABA‑B agonist, accumulates gradually, which is why titration over weeks is standard for long‑term control. In contrast, tizanidine’s alpha‑2 agonism offers a rapid onset but introduces hepatic considerations that the article flags correctly. The side‑effect matrix also reveals a pattern: agents that act centrally (baclofen, diazepam) tend to cause sedation and potential dependence, while peripheral‑acting compounds (methocarbamol) are milder but slower. Moreover, the withdrawal risk associated with baclofen cannot be understated; abrupt cessation may precipitate seizures, a fact that even seasoned clinicians sometimes overlook. The table’s omission of a clear tapering schedule for baclofen is a notable gap. Equally, the discussion around gabapentin’s renal clearance provides a helpful cue for patients with compromised liver function, but it fails to address dose adjustments in chronic kidney disease. The article’s recommendation to combine low‑dose baclofen with a short‑acting agent like tizanidine is plausible, yet it should be tempered by the possibility of additive hypotension. Regarding cost, generic baclofen remains inexpensive, but insurance formularies can favor newer agents, influencing real‑world adherence. Finally, the non‑pharmacologic adjuncts-physical therapy, ergonomics-are mentioned but deserve a stronger presence, as they often determine whether medication alone suffices. In sum, while the guide is thorough, clinicians should supplement it with individualized taper plans, liver/kidney monitoring protocols, and a robust rehab strategy to optimize outcomes.
Lily Saeli
October 15, 2025 AT 07:23Choosing a drug without considering the moral cost to your body is simply irresponsible.
andrew bigdick
October 15, 2025 AT 18:30Just to add a nuance, the speed at which baclofen reaches steady‑state can vary based on individual metabolism, so patients might feel the full benefit a bit later than the typical 2‑4 hours mentioned.
Shelby Wright
October 16, 2025 AT 04:13Wow, nice moral lecture-so original, right? Meanwhile, I’m over here wondering if anyone even reads the fine print about liver toxicity.
Ellen Laird
October 16, 2025 AT 12:33Thsi artcile does a greaat job at listng the side efffects, but the formating could be bettter. Also, the info on cyclobenzaprine’s cardiac risk is a bit thin.
rafaat pronoy
October 16, 2025 AT 19:30Nice overview! 👍 I’m a fan of the baclofen‑tizanidine combo for flare‑ups, just remember to keep an eye on blood pressure.
sachin shinde
October 17, 2025 AT 01:03While the content is useful, there are several grammatical slip‑ups throughout-e.g., “it’s” is used where “its” is intended, and periods are missing after bullet points.
Leon Wood
October 17, 2025 AT 05:13Great read! If you’re hesitant about sedation, start low with methocarbamol and watch how you feel before upping the dose.
George Embaid
October 17, 2025 AT 08:33From a cultural standpoint, it’s worth noting that access to some of these meds varies globally; in many regions, baclofen might be the only affordable option.
Meg Mackenzie
October 17, 2025 AT 11:20Honestly, the pharma industry pushes baclofen as a miracle cure while conveniently hiding the blackout‑risk data-don’t trust the surface narrative.
Shivaraj Karigoudar
October 17, 2025 AT 13:50In terms of pharmacokinetics, baclofen exhibits a bioavailability of approximately 70‑80%, with renal clearance accounting for the majority of excretion; thus, dose adjustments are imperative in patients with glomerular filtration rates below 30 mL/min. Conversely, tizanidine undergoes extensive hepatic metabolism via the CYP1A2 pathway, which introduces potential drug‑drug interactions with common antibiotics and oral contraceptives. The article could enhance its utility by presenting a decision tree that incorporates these metabolic pathways alongside comorbidity profiles, allowing clinicians to rapidly visualize the optimal therapeutic pathway.
Fabio Max
October 17, 2025 AT 16:03Sounds solid-good balance of info and practicality.
Darrell Wardsteele
October 17, 2025 AT 18:00There are numerous spelling errors; e.g., "spasticty" should be "spasticity". Also, the table lacks proper alignment, making it hard to read.
Madeline Leech
October 17, 2025 AT 19:40Anyone still debating baclofen’s safety is living in denial-look at the seizure reports when you pull the plug too fast.
BLAKE LUND
October 17, 2025 AT 21:03Well said! It’s crucial we keep the conversation honest and not let corporate PR gloss over real risks.